Insulin Resistance: Causes, Symptoms and How to Improve It
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — January 2026
In this short video, Dr Sultan Linjawi explains insulin resistance in simple, practical terms — what it is, how it develops, and why it matters for prediabetes and type 2 diabetes.
Insulin resistance — explained simply
Insulin resistance means your muscle, liver, and fat cells stop responding to insulin as efficiently as they should. Your pancreas can often “compensate” for years by producing more insulin — until it can’t keep up, and blood glucose begins to rise.
Why it matters
Insulin resistance is one of the earliest drivers of prediabetes and type 2 diabetes, and it’s closely linked with belly fat (visceral fat), fatty liver, and metabolic syndrome. Understanding it helps explain why weight gain around the middle, rising sugars, fatigue, and increasing medication needs often appear together.
What helps most
- Modest, sustained weight loss (even 5–7% can be meaningful for insulin sensitivity)
- Regular movement (walking + resistance training is a powerful combination)
- Reducing refined carbs and increasing protein + fibre (so hunger is easier to manage)
- Better sleep (sleep restriction and sleep apnoea worsen insulin resistance)
- Stress reduction (chronic stress hormones push glucose up and drive cravings)
Start where you are
If you’re here for a specific question, use this quick guide:
- If you want the full explanation first → What Is Insulin Resistance? A Simple Guide to How It Works and Why It Matters
- If you’re here for symptoms → Symptoms of Insulin Resistance: Early Warning Signs You Shouldn’t Ignore
- If you’re here for testing → How to Test for Insulin Resistance: The Complete Evidence-Based Guide
- If you’re here for weight & belly fat → Insulin Resistance & Weight Gain: Why Belly Fat Matters (Visceral Fat Explained)
- If you’re here for women / PCOS / menopause / pregnancy → Insulin Resistance in Women: PCOS, Menopause and Pregnancy Explained
- If you’re here for causes → What Causes Insulin Resistance? Understanding Why It Develops
- If you’re here for health risks → Health Risks of Insulin Resistance: From Fatty Liver to Heart Disease
- If you’re here for what to do next → How to Reduce Insulin Resistance and Increase Insulin Sensitivity
- If you’re here for diet → Best Diet for Insulin Resistance: What to Eat to Improve Insulin Sensitivity
Prefer to watch first? The video above covers the core “lock and key” concept, then you can dive into whichever section fits your situation.
How is insulin resistance diagnosed
Insulin resistance is diagnosed by a blood test that measures either the fasting insulin level in the morning or by measuring glucose and insulin levels as part of a glucose tolerance test. Testing for insulin resistance is not always done and a diagnosis can be made based on the certain features that a person may demonstrate.
Insulin Levels
| Fasting | 2 hour GTT | |
|---|---|---|
| Normal | less than 10 | less than 60 |
| Inconclusive | 10-20 | 60-100 |
| Insulin Resistant | more than 20 | more than 100 |
Insulin resistance occurs before a person develops type 2 diabetes, when they have borderline diabetes (impaired glucose tolerance) as well as when type 2 diabetes exists.
Features associated with insulin resistance include:
- weight gain around the abdomen
- skin tags
- acanthosis nigricans
- thickened skin
- irregular periods if associated with PCOS (polycystic ovarian syndrome)
- features consistent with endocrine conditions such as acromegaly and Cushing's syndrome
Skin Tags
Skin tags are often associated with insulin resistance and metabolic syndrome, and are frequently seen in obese patients and in patients with diabetes mellitus.
Skin tags are an outgrowth of normal skin. They usually occur in sites of friction, particularly the armpit, neck, under breasts, and in the groin.
Skin tags are diagnosed based upon clinical appearance and treatment is recommended if the skin tags are irritating or removal is desired for cosmetic reasons.


Acanthosis Nigricans
Acanthosis nigricans is characterized by velvety, hyperpigmented plaques on the skin. Like skin tags, acanthosis nigricans is commonly found in areas of the body where two skin areas rub together, including the neck, arm pits, under breasts, and the groin.
Obesity and diabetes are the most common medical disorders linked with acanthosis nigricans, where insulin resistance is likely responsible for the development of acanthosis nigricans.


Polycystic Ovarian Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is the most common cause of infertility in women. It frequently manifests during adolescence, and is primarily characterized by ovulatory dysfunction and hyperandrogenism (high levels of androgens, which are steroid hormones for example testosterone).
PCOS is associated with a number of varied clinical features, including:
- Cutaneous signs of hyperandrogenism (eg, hirsutism, moderate-severe acne)
- Menstrual irregularity (eg, oligo- or amenorrhea, or irregular bleeding)
- Polycystic ovaries (one or both)
- Obesity and insulin resistance
The diagnosis of PCOS has lifelong implications with increased risk for metabolic syndrome, type 2 diabetes mellitus, and, possibly, cardiovascular disease and endometrial carcinoma (cancer) (Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis).
PCOS is associated with insulin resistance and high insulin levels. Obesity and clinical manifestations of insulin resistance, for example skin tags and acanthosis nigricans, are strongly associated with PCOS. Adolescents with PCOS are at an increases risk for glucose intolerance and type 2 diabetes and approximately 10% of women with PCOS will have type 2 diabetes by 40 years.
How this page fits into your learning
My Health Explained is designed to help you understand diabetes over time, not all at once. Most people arrive with one specific question, then build confidence as new questions come up.
This page covers one important part of that picture. You'll see links throughout to related topics that explain why things happen, what options exist, and what tends to help in real life.
If you'd like a broader overview first, start here: Signs and Symptoms of Prediabetes.
If something here raises a question, follow the links that feel most relevant and ignore the rest for now. This resource is built to support learning at your own pace.
Want new articles and practical guides as we publish them? Subscribe to the newsletter.
Free Diabetes Masterclass
Learn proven strategies from Dr Sultan Linjawi to take control of your health.
Learn moreInsulin resistance, Prediabetes (borderline diabetes), and Type 2 Diabetes Mellitus
Insulin resistance may be the best predictor for type 2 diabetes. Before someone is diagnosed with type 2 diabetes, they may be diagnosed with Prediabetes.
Beginning with prediabetes, type 2 diabetes is a progressive disease that develops over many years. It is also a complex condition, affecting many parts of your body. When people are diagnosed with type 2 diabetes mellitus, the disease process may have been present for 5-10 years. This means some complications may already be present at diagnosis.
What is Prediabetes, also known as borderline diabetes?
Prediabetes is a condition that describes a person who has a number of abnormal glucose blood tests suggesting they have borderline diabetes. It may also be called “impaired glucose tolerance” or “metabolic syndrome”. People with prediabetes are very likely to progress to developing type 2 diabetes in the coming few years. More importantly, people with prediabetes are the most likely to recover and return back to normal by making a few important changes.
What is metabolic syndrome?
Metabolic syndrome, sometimes called syndrome X, is a collection of disorders, including high blood pressure, insulin resistance, abnormal cholesterol levels, and excess fat around the waist. People with metabolic syndrome are twice as likely to have a heart attack and stroke, and five times more likely to develop type 2 diabetes, compared to people without metabolic syndrome.

Over the past three decades, the prevalence of Metabolic Syndrome has increased. Did you know that children and adolescents can also have metabolic syndrome? It’s not just adults! More and more young people are showing signs of metabolic syndrome. The incidence of metabolic syndrome often parallels the incidence of type 2 diabetes and obesity (The Global Epidemic of the Metabolic Syndrome). According to the Centers for Disease Control and Prevention (CDC), 12.2% or 30.2 million adults (aged 18 years and older) in the USA had type 2 diabetes in 2017. What’s scary, is that a quarter of these adults, don’t even realise that they have diabetes.
Typically, adults with type 2 diabetes will present with comorbidities such as obesity, hypertension (high blood pressure), and dyslipidemia (elevated cholesterol and fats in the blood). A comorbidity is the presence of one or more additional diseases or disorders. Other comorbidities that may be present at diagnosis or can develop over time, include gum disease, sleep apnoea, fatty liver disease, depression and anxiety, and bone fractures (Comprehensive Medical Evaluation and Assessment of Comorbidities by the American Diabetes Association).
If there are any complications present in a person with diabetes, the disease progression can be slowed by interventions, for example better management of blood glucose levels, blood pressure, and blood lipids.
What is Type 2 Diabetes?
Type 2 diabetes explained simply
Like prediabetes, Type 2 diabetes is an elevation in blood sugars that occurs when glucose can’t get into your fat and muscles where it is needed. Elevated blood glucose damages the lining of blood vessels leading to a range of complications in various organs of the body.
Type 2 diabetes explained in detail
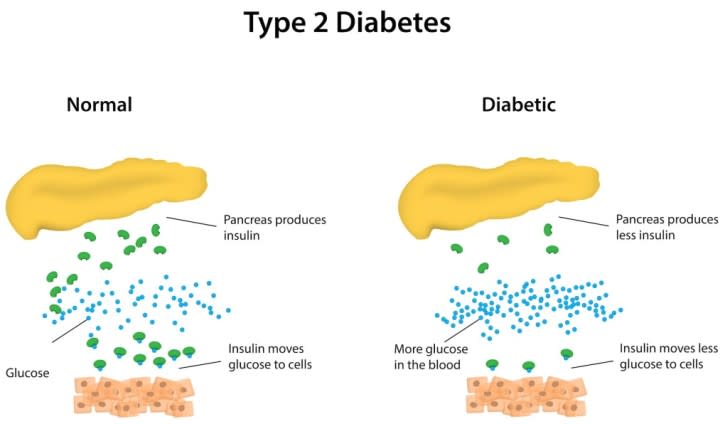
Type 2 diabetes is rapidly becoming of the most common long-term disease in the world. The problem causing an elevation in the blood glucose levels occurs when there is a change in the shape of the insulin receptor. In the normal situation, the body produces a small chemical called insulin (key) whose purpose is to bind to a receptor (lock) on the surface of fat and muscle cells, opening a channel to allow glucose to enter those cells. In type 2 diabetes the shape of this receptor changes mostly as a consequence of weight gain around the stomach. As we have discussed, the process of the lock changing shape is called Insulin Resistance.
Type 2 diabetes is a progressive disease. If left untreated, the pancreas will begin to fail and no longer be able to produce insulin, contributing to the increased glucose levels in the blood.
Symptoms of Type 2 diabetes
In diabetes mellitus, symptoms that you experience are related to:
a) the severity of diabetes, i.e. how high your blood glucose levels are,
and
b) how long you have had the condition, i.e. how long you have had high blood glucose levels for.
In people with type 2 diabetes, the progression of the condition happens much more slowly, over the course of several years, so the symptoms happen slowly and are often subtle. You may not even notice anything at all, or you may even dismiss them as a normal part of growing older.
By the time that you notice something isn’t quite right, you could have been experiencing high blood glucose levels for years! Often people who are diagnosed with type 2 diabetes, have had diabetes for perhaps 5 years and borderline diabetes for many years before that.
What is the most common symptom in people with type 2 diabetes?
The most common sign of diabetes is…
Nothing.
That’s right. Nothing. The reason that doctors need to test for diabetes (and people need to demand it), is that most people have no idea that they have it. This regular testing is most important in people at the highest risk of developing diabetes.
If you want to learn how type 2 diabetes mellitus can affect men and women differently, we can also written dedicated articles to answer your questions:
Dr Sultan also has a helpful video discussing the symptoms of diabetes. To learn more, watch the What are the symptoms of diabetes? video.
Type 2 diabetes complications
Diabetes is a vascular disease which means it affects blood vessels. Complications in type 2 diabetes can be described as microvascular (small blood vessels) or macrovascular (large blood vessels) complications (Microvascular and Macrovascular Complications of Diabetes). Diabetes-related complications occur over time due to persistent high blood glucose levels, high blood pressure, and abnormal cholesterol levels. These complications are serious and can be life-threatening.
Macrovascular complications - Problems with large blood vessels
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- Coronary artery disease which can lead to a heart attack
- Cerebrovascular disease which can lead to a stroke
- Peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity as well as amputations.
Microvascular complications – problems with small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 2 diabetes. Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Hb A1c and complications in type 2 diabetes
Higher Hb A1c readings are also linked to an increased risk of complications. You can read about Hb A1c and the risk of developing type 2 diabetes complications to learn more.
What is insulin resistance?
Insulin is a hormone that acts like a key. It unlocks receptors on muscle and fat cells, allowing glucose to move from the bloodstream into the cell, where it can be used for energy or stored for later.
When someone develops insulin resistance, the “lock” on the cell surface changes shape. The key still works — but only if the pancreas produces much more insulin. This results in a period of hyperinsulinemia (high insulin levels) long before glucose levels rise.
Over time, the pancreas struggles to keep up. When it can no longer produce enough insulin to overcome the resistance, blood glucose begins to rise, first into the prediabetes range and later into the type 2 diabetes range.
This process may begin 5–10 years before a diagnosis — which is why early recognition matters.
Trusted overviews from the NIDDK and CDC confirm this stepwise progression.
Frequently Asked Questions
What is insulin resistance?
Insulin resistance occurs when the body’s tissues – especially muscle, liver, and fat – do not respond properly to insulin. To keep blood glucose in a safe range, the pancreas has to produce more and more insulin. A simple way to picture this is that insulin is the “key” and the receptor on the cell surface is the “lock”; when insulin resistance develops, the lock no longer opens easily, so glucose cannot enter the cells as well as it should.
What is insulin?
Insulin is a hormone produced by the beta cells in the pancreas. It acts like a key that binds to receptors on fat and muscle cells, allowing glucose to move from the bloodstream into the cells to be used for energy or stored for later. Without enough insulin – or if the body becomes resistant to it – blood glucose levels can rise.
What are the causes of insulin resistance?
The most common cause of insulin resistance is excess body weight, particularly visceral fat around the abdomen. Other contributing factors include ageing, polycystic ovary syndrome (PCOS), chronic stress, certain medications such as steroids, pregnancy, lipodystrophy, and the presence of insulin antibodies. Family history and genetics also play an important role in how likely you are to develop insulin resistance.
What are the complications of insulin resistance?
Insulin resistance is a key driver of many metabolic conditions. Over time it is associated with impaired fasting glucose, impaired glucose tolerance, prediabetes, and type 2 diabetes. It can also worsen insulin requirements in people with type 1 diabetes and is linked to coronary artery disease, metabolic syndrome, polycystic ovary syndrome, and non-alcoholic fatty liver disease (NAFLD).
What are the risk factors for developing insulin resistance?
Some risk factors for insulin resistance cannot be changed and some can. Non-modifiable risks include family history of type 2 diabetes, genetic background, age, and sex. Modifiable risk factors include excess abdominal weight, high blood pressure, high cholesterol or triglycerides, physical inactivity, and a diet high in refined carbohydrates, added sugars, and saturated fats.
Can insulin resistance be reversed or improved?
Yes. Insulin resistance can often be improved – and sometimes substantially reversed – with sustained lifestyle changes. Gradual weight loss, increased physical activity, better sleep, and a healthier eating pattern all help the body’s cells respond more effectively to insulin. As fat cells shrink and inflammation falls, insulin signalling improves and blood glucose levels usually follow.
What can I do to reduce insulin resistance?
Practical steps to reduce insulin resistance include:
- Aiming for gradual, sustained weight loss if you are above your healthy weight.
- Doing regular physical activity that combines aerobic exercise (for example walking, cycling, swimming) and resistance training (such as weights or body-weight exercises).
- Choosing a high-fibre, minimally processed eating pattern with fewer refined carbohydrates and sugary drinks.
- Prioritising good-quality sleep and managing stress.
- Working with your doctor, diabetes educator, or dietitian for personalised advice and monitoring.
How is insulin resistance diagnosed?
There is no single blood test used everywhere to diagnose insulin resistance. Doctors may use fasting insulin and glucose levels, or take glucose and insulin measurements during an oral glucose tolerance test (OGTT). They also look at clinical features such as central weight gain, acanthosis nigricans (dark, velvety skin around the neck or armpits), skin tags, blood pressure, cholesterol, and triglycerides. The exact testing approach can vary between clinics and countries.
What features are associated with insulin resistance?
Common features that suggest insulin resistance include increased abdominal (belly) fat, skin tags, and acanthosis nigricans – a darkened, velvety thickening of the skin, often around the neck, armpits, or groin. Irregular menstrual cycles and symptoms of polycystic ovary syndrome (PCOS) in women are frequently linked to insulin resistance. Certain hormonal conditions such as acromegaly and Cushing’s syndrome are also associated with marked insulin resistance.
Is insulin resistance related to prediabetes and type 2 diabetes?
Yes. Insulin resistance is a major underlying cause of both prediabetes and type 2 diabetes. The process usually develops gradually over many years. At first, the pancreas can compensate by producing more insulin, but over time this compensation fails and blood glucose levels begin to rise. Type 2 diabetes may be present for a long time before it is diagnosed, which is why early lifestyle changes and screening are so important.
What is prediabetes?
Prediabetes describes blood glucose levels that are higher than normal but not yet in the diabetes range. It is often labelled as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT). Prediabetes is a warning sign that insulin resistance is already present. The good news is that many people with prediabetes can return to normal glucose levels with sustained lifestyle changes such as healthy eating, weight loss, and regular physical activity.
What is metabolic syndrome?
Metabolic syndrome, sometimes called syndrome X, is a cluster of risk factors that tend to occur together. These include central obesity (increased waist circumference), insulin resistance, high blood pressure, elevated triglycerides, and low HDL (“good”) cholesterol. Having metabolic syndrome significantly increases your risk of heart disease, stroke, and type 2 diabetes.
What is type 2 diabetes?
Type 2 diabetes is one of the most common long-term conditions worldwide. It develops when insulin resistance and a gradual decline in insulin production combine to cause persistently high blood glucose levels. Early on, lifestyle changes such as improved diet, weight loss, and increased physical activity can make a big difference. Over time, many people also need medications – and sometimes insulin – to keep blood glucose within a safe range.
Video Transcript
So one of the things that happens to people with Type 2 diabetes or people with pre-diabetes or borderline diabetes is a long time before developing the condition they develop a thing called insulin resistance.
If you have an interest in diabetes and you want to keep up to date then subscribe, share, comment and like this page.
I want to explain a little bit about how insulin resistance works and why it occurs because I think there are a few important aspects that are worth knowing about. So with everything with diabetes we really start with food. If that food is excessive to our current needs we will break it down and we will store it inside a fat cell. And the way that we get particularly carbohydrates into fat cell is there is a lock on the surface of the cell called the insulin receptor. So when insulin as a lock binds to insulin which is like a key the two bind together and that actually opens a channel that allows food to get into the cell. Now if we eat excessive amounts of food then what will typically happen is that fat cell will increase in size.
If we continue to eat excessive amounts of food then that fat cell will get bigger and bigger and bigger. And eventually it will get to the point that even if the fat cell wants to just keep on growing it is constrained by its physical size, it cannot just get bigger. And at that point the fat cell is in trouble. Because it has to find a way to prevent excessive amounts of energy particularly in the form of glucose and carbohydrate from getting into the fat cell. And the way that is occurring is it changes the shape of the lock and you create this process of insulin resistance. Your fat cells become resistant to the effect of insulin so you produce a large amount of insulin just to try to open that lock.
Now over time what happens is the pancreas produces extra insulin and then eventually it cannot continue to produce the high amounts of insulin that it needs and the pancreas starts to fail and specifically the pancreatic insulin production starts to fail and the blood sugars rise.
Can insulin resistance be changed?
Well the answer is if you lose weight and you shrink your fat cell and you continue to shrink the fat cell then eventually what will happen is the lock will go back to normal and the insulin will be able to fit nicely.
And so when people talk about reversing diabetes they are really talking about sustained weight reduction that leads to improvement of the shape of the lock.
Now it may be that the pancreatic function by the time a person decides that they really want to deal with their diabetes is so diminished that they are not going to be able to produce enough insulin even with a well working lock. But nonetheless if you can reduce insulin resistance there really is quite a profound improvement in glucose levels that a person can expect and the earlier that you deal with insulin resistance the better.
If you found this video helpful then please subscribe to the channel so that I can keep you up to date as all the new videos come online.
Insulin resistance is one of the earliest and most important steps in the journey toward prediabetes and type 2 diabetes. It often develops silently for many years before blood glucose levels rise. Understanding what it is, why it happens, and how to improve it is one of the most powerful things you can do to protect your long-term health.
In the short video below, Dr Sultan Linjawi explains insulin resistance in simple, visual terms — using the “lock and key” analogy that helps make sense of how fat cells change and why glucose can no longer enter as easily.
What causes insulin resistance?
The most common driver is weight gain around the abdomen, but many other factors can contribute. These are grouped into modifiable and non-modifiable risks.
Non-modifiable risk factors
- Family history of type 2 diabetes
- Genetics
- Ageing
- Certain ethnic backgrounds
Modifiable risk factors
- Excess abdominal fat (visceral fat)
- Physical inactivity
- Poor sleep quality or sleep apnoea
- High levels of stress
- Diets high in refined carbohydrates and saturated fats
- Certain medications (e.g., steroids)
Medical conditions closely linked with insulin resistance include metabolic syndrome, fatty liver disease, PCOS, and type 2 diabetes.
For clinicians and patients who want deeper detail, the NIDDK summary of causes and mechanisms is an excellent reference.
What are the signs of insulin resistance?
Most people have no symptoms at all. But some physical signs can offer clues:
- Acanthosis nigricans – dark, velvety patches around the neck or underarms
- Skin tags
- Increased waist circumference
- Fatigue
How is insulin resistance diagnosed?
There is no single routine test. Healthcare professionals may assess clinical features plus:
- Fasting glucose and insulin levels
- Oral glucose tolerance test (OGTT)
- HbA1c
- Lipid panel (high triglycerides and low HDL can be clues)
Insulin resistance matters because it is the earliest driver of:
Can insulin resistance be improved or reversed?
Yes — for many people, insulin resistance is highly responsive to lifestyle changes. Evidence from large trials such as the Diabetes Prevention Program (DPP) shows that weight loss of just 5–7% can significantly improve insulin sensitivity and lower the risk of diabetes.
Evidence-based ways to improve insulin resistance
- Weight reduction — even modest loss shrinks fat cells and helps the insulin “lock” return to normal shape
- Regular movement — walking + resistance training improves muscle glucose uptake
- Improved sleep and reduced stress
- Metformin — recommended in some cases (e.g., PCOS, prediabetes with high risk)
Understanding insulin resistance is the first step. Taking action is the next.
Want guided support? Our free webinar explains insulin resistance, prediabetes, and early type 2 diabetes — and the key steps that genuinely move the needle.