What are the risk factors of developing type 1 diabetes?
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — December 2025

Type 1 diabetes risk factors
Type 1 diabetes typically develops when the immune systems destroys the insulin-producing cells of the pancreas, called the beta cells. This process is called an autoimmune response and occurs in many different disease processes leading to destruction or stimulation of many different organs. Often the body's immune system is triggered to attack something like a virus - called the environmental insult - but then creates antibodies that attack the body itself by accident.
It is not clearly understood what the cause is for type 1 diabetes, but there are some factors that may increase a person’s likelihood of developing the condition. This can include their genetics and whether close family members are diagnosed with type 1 diabetes, as well as the influence of other autoimmune diseases and environmental factors.
Type 1 Diabetes Content |
|---|
| Type 1 Program |
| Overview |
| Risk Factors |
| Symptoms |
| Diagnosis |
| Complications |
| Treatment |
| Diet |
| Monitoring |
| Tools |
| Mental Health |
| Prevention |
GENETICS+ENVIROMENTAL = HIGH RISK OF CONDITION
Who is at risk of type 1 diabetes?
The simple answer: anyone. Although it is more likely if someone in your family has type 1 or perhaps another autoimmune disease like coeliac disease, Addison's disease, pernicious anaemia or autoimmune thyroid disease. All these suggest a genetic risk is present.
It can occur at any age but typically doesn’t develop in the first year of life when the immune system is still underdeveloped. Even though it is often associated with children, half the people who develop type 1 are over the age of 30.
There have been studies which have aimed to link genetics and environmental factors with the rates of type 1 diabetes.
Genetic susceptibility
Type 1 diabetes can occur in people with a family history of type 1 diabetes, but it can also develop in people who do not have a family history of diabetes.
The risk of developing of type 1 diabetes is increased in those who have close relatives of a person with type 1 diabetes (ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents). These include:
- no family history – 0.4 percent
- child of a mother with type 1 diabetes – 1 to 4 percent
- child of a father with type 1 diabetes – 3 to 8 percent
- child of both parents with type 1 diabetes – report as high as 30 percent
- sibling (not a twin) of affected patient – 3 to 6 percent by age 20 years and 10 percent by 60 years
- nonidentical twin – 8 percent
- identical twin – 30 percent within 10 years of diagnosis of the first twin and 65 percent concordance by age 60 years
Studies in the United States has found that there are ethnic differences in the rates of type 1 diabetes (Prevalence of Type 1 and Type 2 Diabetes Among Children and Adolescents From 2001 to 2009). In 2009, a study looked at large multi-ethnic populations, which showed the highest prevalence was seen in non-Hispanic white youth, followed by African American, Hispanic, Asian-Pacific Islanders, and American Indians.
Autoimmunity
The main role of the immune system is to fight off foreign invaders, for example bacteria or viruses. In autoimmune conditions, the body’s own immune system attacks healthy cells, tissues, or organs, which can result in inflammation and damage. Along with type 1 diabetes, there are over 80 autoimmune diseases. There are some more common (i.e. diabetes, rheumatoid arthritis) than others (i.e. lupus, vasculitis).
For people who have an autoimmune disease, they are at an increased risk of developing other autoimmune conditions. So, if you have type 1 diabetes, then you are susceptible to another autoimmune disease (Type 1 Diabetes and Autoimmunity). This also means that if you don’t have type 1 diabetes, but you have another autoimmune condition, you are susceptible to developing type 1 diabetes. The most common autoimmune diseases that are associated with type 1 diabetes is coeliac disease and Hashimoto's thyroiditis.
Hashimoto's Thyroiditis
Approximately 2-5 percent of people with type 1 diabetes have an underactive thyroid and are called hypothyroid. Up to 20 percent of people with type 1 diabetes have positive antithyroid antibodies that can be measured in the blood (Thyroid Autoimmunity in Children and Adolescents With Type 1 Diabetes). Many people with antithyroid antibodies will go on to develop an autoimmune underactive thyroid called Hashimoto's thyroiditis.
It is suggested that children and adolescents with type 1 diabetes should be screened for autoimmune thyroiditis. If thyroid stimulating hormone (TSH) levels are normal, it is suggested that screening should take place every 1-2 years as they develop an undeactive thyroid in the future.
Graves Disease (Thyrotoxicosis)
Whilst people with Hashimoto's disease develop an underactive thyroid, another group of people can produce antibodies that attack and stimulate the thyroid. This is called Graves disease. People with Graves disease can develop an overactive thyroid requiring treatment.
Coeliac Disease
Coeliac disease is an autoimmune condition where antibodies attack the lining of the upper part of the gut(small intestine) leading the a change in the structure that leads to an inability to absorb certain nutrients. The production of these antibodies is due to a genetic susceptibility and enviromental insult. This insult is a gluten, a plant based protein found in many grains and seeds.
Approximately 5 percent of people with type 1 diabetes have coeliac disease and most cases of coeliac disease are diagnosed within five years of diabetes onset (Screening for Celiac Disease in Type 1 Diabetes: A Systematic Review). As with thyroiditis, it is also suggested that children and adolescents are screened for coeliac disease. If screening for coeliac disease is negative, then patients should be re-screened every 2 years, or whenever the person starts to exhibit signs of coeliac disease.
Environmental factors
The influence of the environment around us is another important factor in the development of type 1 diabetes. Studies have looked at the role of viruses and diet.
The role of viruses
The link between viruses and the development of type 1 diabetes is interesting. Some studies have found that exposure to enteroviruses (a common type of virus), both while in the uterus and during childhood, may lead to damage to the insulin producing cells of the pancreas causing diabetes.
One study has found that viruses can cause diabetes either by directly infecting and destroying the beta cells of the pancreas, or by triggering an autoimmune attack against these cells in animal models (Diabetes mellitus due to viruses--some recent developments). What’s interesting about this, is that another study has found the opposite. It was found that viruses may be protective against type 1 diabetes (Prevention of type I diabetes in non-obese diabetic mice by virus infection). Again, this was conducted in animal models.
The role of diet in causing type 1 diabetes
Cow’s milk
It is believed that there are several dietary factors that may influence the development of type 1 diabetes. There has been a lot of focus on cow’s milk (Diet, cow's milk protein antibodies and the risk of IDDM in Finnish children. Childhood Diabetes in Finland Study Group). This Finnish study suggested that there is an association with the introduction to cow’s milk dairy products at an early age and high milk consumption during childhood, with an increase in the risk of type 1 diabetes. However, there have been some other studies that have debunked this finding. There was a cross-sectional study that found no evidence of an association between early exposure to cow’s milk and the development of type 1 diabetes (Lack of Association Between Early Exposure to Cow's Milk Protein and β-Cell Autoimmunity – Diabetes Autoimmunity Study in the Young (DAISY)).
Cereals
Studies have examined the link between the timing of initial exposure to cereals and the risk of developing type 1 diabetes. Two studies have found that newborns who are at a high risk of developing type 1 diabetes, found that exposure to cereals before the age of 3 months or after 7 months was associated with an increased risk of developing type 1 diabetes compared with infants who were exposed to cereal between the ages of 4-6 months (Timing of Initial Cereal Exposure in Infancy and Risk of Islet Autoimmunity). Current infant feeding guidelines suggest that cereals should be introduced between the ages of 4-6 months, so there is no need to go against these current guidelines.
What are the symptoms of type 1 diabetes?
If you have any family members who have type 1 diabetes, you may be at an increased risk of developing the condition yourself. If you start to experience any of the following symptoms, you should go to your doctor and ask to be tested.
Most people with type 1 diabetes have symptoms of high blood glucose levels (hyperglycaemia). Symptoms of hypoglycaemia can include:
- excessive thirst
- frequent urination
- feeling tired
- increased hunger
- unintentional weight loss
- blurred vision
- frequent yeast infections or urinary tract infections
- slow healing wounds
You can learn more about the symptoms of type 1 diabetes in our article What are the symptoms of type 1 diabetes?
What to do if you think you might have type 1 diabetes?
If you suspect you may have type 1 diabetes is to visit your doctor and request a blood test. Once diagnosed it is very important to get educated!! When you know what is happening and what to do, you can get back to feeling good again.
What should I do next?
If you experience any symptoms of type 1 diabetes or you have risk factors for developing type 1 diabetes, it is important to get tested for as soon as possible. Some people are at higher risk and need regular testing.
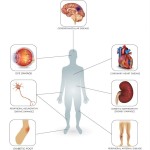
By diagnosing and treating the type 1 diabetes early, it means you can decrease the risk of developing or delay any further health complications of type 1 diabetes, for example nerve damage, blindness, and heart disease. It is important to know that diagnosing type 1 diabetes should not rely solely on using a Hb A1c test.
Once you learn what your type 1 diagnosis is, or if you already have type 1 diabetes, the next most important step is to become educated. You can join the 12-week Type 1 Diabetes Program to help you learn how best to manage the condition. For example, you can learn how best to monitor blood glucose levels in type 1 diabetes. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make. The first week is free and full of helpful and crucial information.
Free Diabetes Masterclass
Learn proven strategies from Dr Sultan Linjawi to take control of your health.
Learn more about this webinar
Loading webinar times...
Interested in more information on type 1 diabetes?
Follow the links below to learn more about type 1 diabetes.
Frequently Asked Questions
What is type 1 diabetes?
Type 1 diabetes is an autoimmune condition where the immune system mistakenly destroys the insulin-producing beta cells in the pancreas. This leads to little or no insulin production. Both genetic susceptibility and environmental triggers contribute to the condition.
Who is at risk of type 1 diabetes?
Anyone can develop type 1 diabetes. Risk increases if you have a family history of type 1 diabetes or if you or your relatives have autoimmune conditions such as coeliac disease, autoimmune thyroid disease, Addison’s disease, or pernicious anaemia. Type 1 diabetes can occur at any age, not just childhood.
How strong is the genetic risk of type 1 diabetes?
Risk varies depending on the family relationship. Approximate lifetime risks include: general population ~0.4%; child of a mother with type 1 diabetes 1–4%; child of a father with type 1 diabetes 3–8%; both parents ~30%; sibling 3–6% by age 20 and ~10% by age 60; identical twin up to ~65% by age 60. These figures reflect genetic susceptibility combined with environmental triggers.
What is autoimmunity in type 1 diabetes?
Autoimmunity occurs when the immune system attacks the body’s own tissues. In type 1 diabetes, immune cells target pancreatic beta cells, reducing insulin production. People with one autoimmune condition have a higher likelihood of developing another, which is why routine screening is often recommended.
How is Hashimoto’s thyroiditis linked to type 1 diabetes?
Hashimoto’s thyroiditis, an autoimmune form of hypothyroidism, is more common in people with type 1 diabetes. Many have detectable antithyroid antibodies, and some develop underactive thyroid. Periodic thyroid testing is recommended as part of routine diabetes care.
How is Graves’ disease linked to type 1 diabetes?
Graves’ disease is an autoimmune form of hyperthyroidism. It occurs more frequently in people with type 1 diabetes and may require medication, radioiodine therapy, or surgery depending on severity.
How is coeliac disease linked to type 1 diabetes?
Coeliac disease is an autoimmune condition triggered by gluten in genetically susceptible individuals. It is significantly more common in people with type 1 diabetes, which is why routine screening is often recommended—especially in children or those with symptoms.
What environmental factors may trigger type 1 diabetes?
Several environmental influences are being studied, including viral infections, early-life nutrition, microbiome changes, and other triggers. These factors likely interact with genetic risk rather than cause type 1 diabetes alone.
What are the symptoms of type 1 diabetes?
Symptoms can develop quickly and may include excessive thirst, frequent urination, fatigue, hunger, blurred vision, unintentional weight loss, and recurrent infections. In some cases, diabetic ketoacidosis (DKA) may be the first presentation.
What should I do if I think I might have type 1 diabetes?
Seek medical attention urgently. Blood tests can confirm the diagnosis. Early detection and immediate insulin therapy are crucial to prevent serious complications such as ketoacidosis.