What are the complications of type 1 diabetes?
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — January 2026

Complications of untreated type 1 diabetes
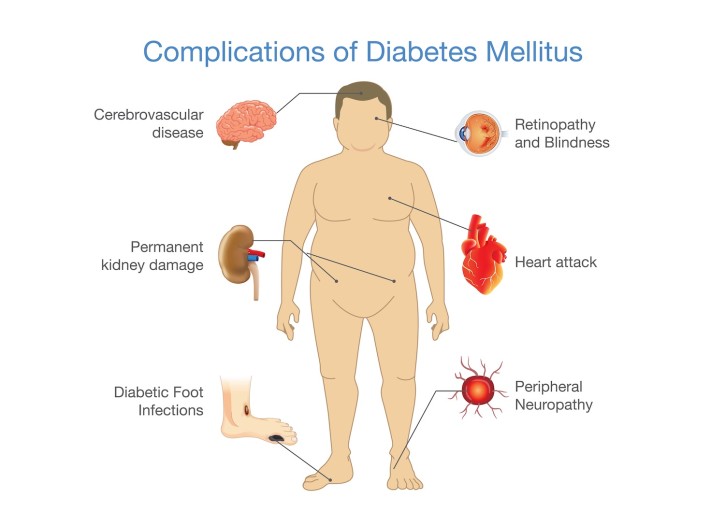
Complications in diabetes are all related to poor blood glucose control. Poor control of blood glucose levels over a number of years can affect the blood vessels in the body, which can result in problems with the small blood vessels (known as microvascular complications) or the large blood vessels (known as macrovascular complications). The effects on the blood vessels from ongoing uncontrolled blood glucose levels, are a major source of morbidity and mortality for people with diabetes (Microvascular and Macrovascular Complications of Diabetes).
Microvascular complications – problems with small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 1 diabetes. Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Type 1 Diabetes Content |
|---|
| Type 1 Program |
| Overview |
| Risk Factors |
| Symptoms |
| Diagnosis |
| Complications |
| Treatment |
| Diet |
| Monitoring |
| Tools |
| Mental Health |
| Prevention |
Retinopathy, nephropathy, and neuropathy are all progressive disorders. These complications won’t be noticeable at the beginning as they don’t produce any symptoms during the early stages. They can also be prevented, or the severity minimized with the combination of regular medical check-ups and adequate blood glucose management. Similar to macrovascular complications, microvascular complications can increase with ongoing poor blood glucose control as well as the duration that you have had diabetes. This means, the longer that you have had diabetes and the longer you have had high blood glucose levels, means that you are more likely to develop diabetes-related complications. So! The earlier that any of these complications are detected, means that early intervention can occur which may be able to reverse any of these microvascular diseases or help to delay further progression.
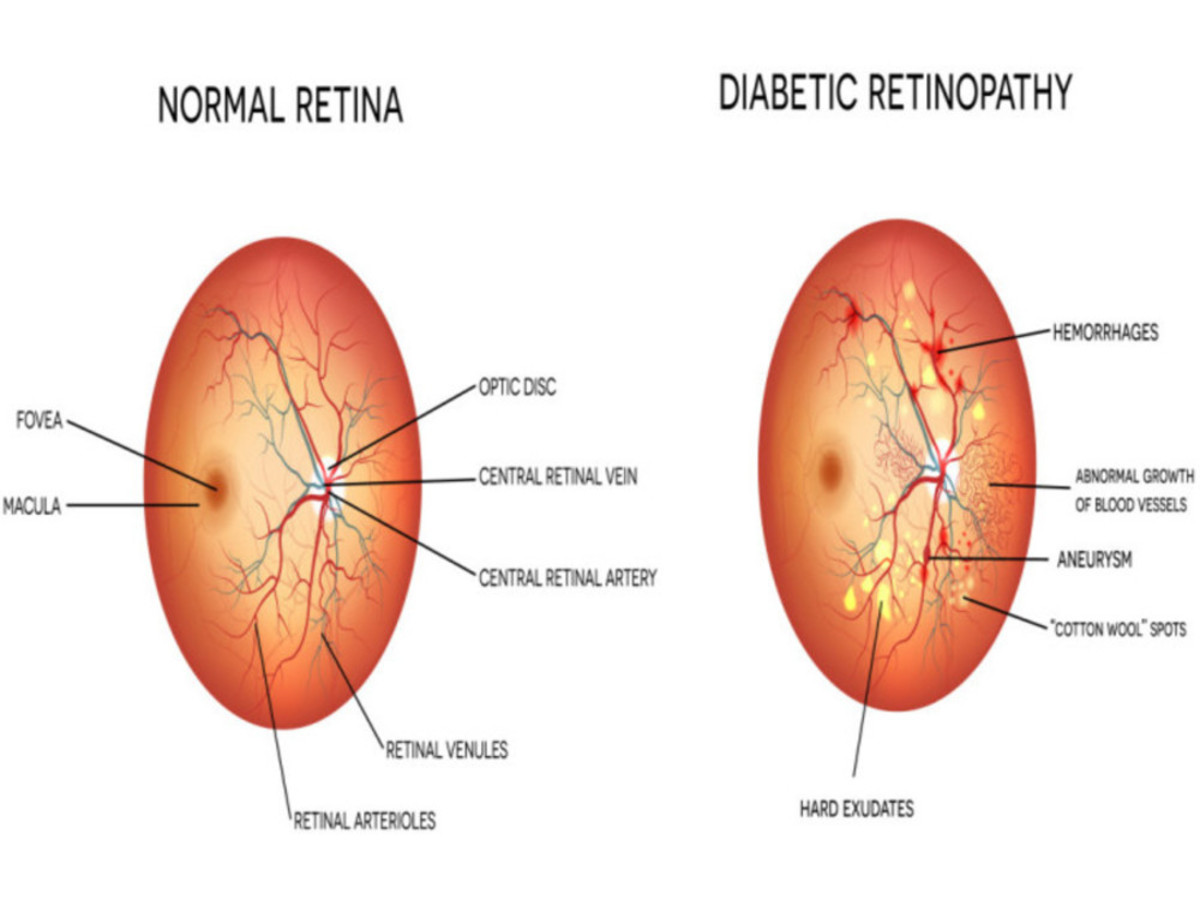
Retinopathy
Eye problems in people with diabetes, is known as diabetic retinopathy. It can lead to loss of vision and even blindness (Diabetic Retinopathy). Retinopathy affects the small blood vessels of the retina at the back of the eye. For most people, retinopathy will have no symptoms until the disease is quite advanced. Unfortunately, by then there is little that can be done about any vision loss. This is why early detection is so important.
Diabetic retinopathy is the most common microvascular complication of diabetes. In the U.K. Prospective Diabetes Study (UKPDS) it was found that most patients with type 1 diabetes, began to develop evidence of retinopathy within 20 years of diagnosis (Clinical Factors Associated With Resistance to Microvascular Complications in Diabetic Patients of Extreme Disease Duration).
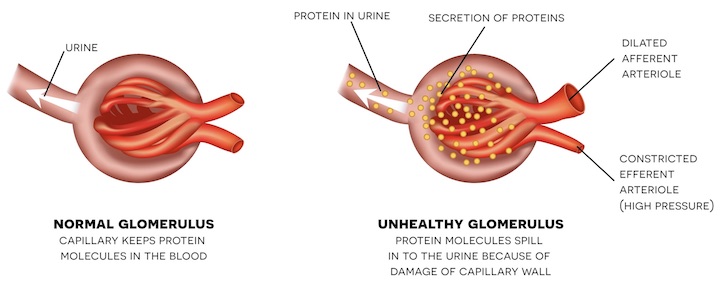
Nephropathy
Did you know that in the United States, diabetic nephropathy is the leading cause of kidney failure? (Microvascular and Macrovascular Complications of Diabetes). Diabetes-related nephropathy affects the small blood vessels in the kidney, which can alter the normal function of the kidney. The kidneys are responsible for filtering our blood and removing any waste products and excess salts and water from our blood. When the kidneys are functioning normally, they prevent protein leaking into our urine. So, if there is protein found in the urine, this is often the first sign of nephropathy.
If you have diabetes, you may not even realise that you have any problems with your kidneys. You may still even be producing normal amounts of urine. But did you know that people with diabetic kidney disease usually don’t exhibit any symptoms until at least 75 percent of the kidneys’ function is lost! (Diabetic Nephropathy: Diagnosis, Prevention, and Treatment.)
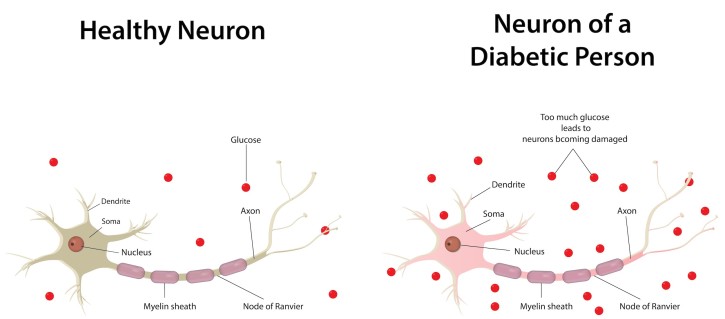
Neuropathy
Diabetes-related neuropathy is also a progressive disorder affecting our nerves. Nerves have important roles in our body, as they act to transmit signals all over our body. Our nervous system has a wide range of jobs including, controlling our heart rate and blood pressure, as well being responsible for nerve conduction and sensory perception.
Diabetic neuropathy can lead to amputations in some people with diabetes. It has been found to be responsible for more than 80% of amputations that occur after a foot injury or foot ulcer, which can result from diabetic neuropathy (The Association Between Cardiovascular Autonomic Neuropathy and Mortality in Individuals with Diabetes).
Macrovascular complications - problems with large blood vessels
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- Coronary artery disease which can lead to a heart attack
- Cerebrovascular disease which can lead to a stroke
- Peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity as well as amputations.
Diabetes increases the risk of that a person will develop cardiovascular disease compared to someone who does not have diabetes. In fact, cardiovascular disease is the primary cause of death in people with type 1 diabetes (The effect of intensive diabetes treatment on resting heart rate in type 1 diabetes: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study).
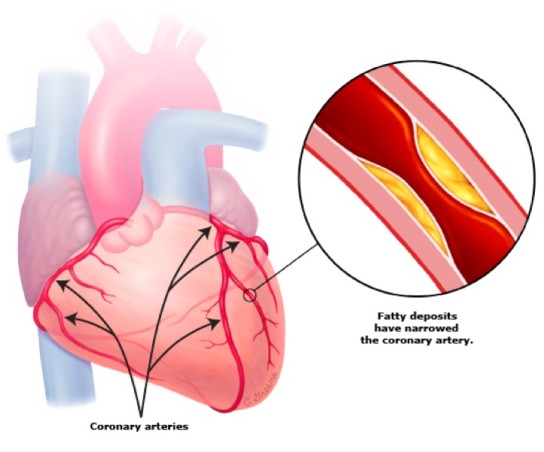
The main cause for these macrovascular diseases is atherosclerosis (Diabetes and atherosclerosis: epidemiology, pathophysiology, and management). Atherosclerosis is a build-up of fatty deposits in the blood vessels, typically the arteries. These fatty plaques can grow over time and result in narrowing of the blood vessels or completely blocking blood flow.
Atherosclerosis can occur anywhere in the body. When it occurs in the arteries of the heart, it is called coronary artery disease. When it occurs in the arteries of the brain, it is called cerebrovascular disease. Finally, when atherosclerosis occurs in the arteries supplying blood to other areas of the body like the legs or kidneys, it is called peripheral artery disease.
Coronary artery disease
Coronary artery disease is a condition that puts you at risk of a heart attack and other forms of heart disease. The coronary arteries supply blood to the heart muscles and when these arteries become narrow due to atherosclerosis, it can lead to a heart attack. Heart disease is actually the number one killer of people with type 1 diabetes (Microvascular and Macrovascular Complications of Diabetes).
Typically, the first sign that someone has heart disease, and even diabetes, is when they have a heart attack. Some people who have heart disease may experience chest pain even if they aren’t having a heart attack. This can happen while they are walking, going up stairs, or just moving around.
It is important to be able to recognise the symptoms of a heart attack. They can include:
- Pain, pressure or discomfort in the centre of the chest
- Pain, tingling or discomfort in other parts of the upper body including the arms, back, neck, jaw, and stomach
- Shortness of breath
- Nausea, vomiting, heartburn, or burping
- Sweating or having cold, clammy skin
- Racing or uneven heartbeat
- Feeling of dizziness or light-headedness
If you experience any of these symptoms for more than 10 minutes, or they keep coming or going, or any pain in your chest you experience is new or different, contact your emergency services for an ambulance right away.
Stroke (cerebrovascular disease)
Cerebrovascular refers to blood flow to the brain. Cerebrovascular disease refers to all disorders whereby the brain is temporarily or permanently affected by inadequate blood flow or bleeding in one or more of the blood vessels to the brain. This may occur due to a stroke or an aneurysm.
One way that blood flow can be restricted to the brain is through narrowing of the blood vessels, for example in the carotid arteries. Blockages in these arteries, severely increases a person’s risk of having a stroke. A stroke is when a part of the brain becomes damaged due to problems with blood flow in the brain.

Blood clots or the fatty plaque deposits can break off and travel to smaller blood vessels in the brain, where it can cause a blockage and lead to a stroke. A stroke may also occur when an artery breaks open causing excessive bleeding into and around the brain.
The lasting effects of the stroke can differ for everyone and can also depend on how quickly you receive treatment and which part of your brain is affected. For some people who have had a stroke, they may recover with only minor problems, but many people have ongoing issues. Following a stroke, some people may be:
- Unable to understand speech or are unable to speak themselves
- Paralysed down one side of the body, including the side of the face, the arm, and the leg
- Unable to take care of themselves, including to dress and feed themselves
If you are unsure of the warning signs of when someone is having a stroke, think of the word “FAST.” Each letter stands for signs to look out for:
- Face – Does the face look uneven or droop on one side?
- Arm – Does the person have weakness or numbness in one or both arms?
- Speech – Is the person having trouble speaking? Does the speech sound strange?
- Time – If you notice any of these signs, it’s time to call the ambulance.
Peripheral artery disease
Peripheral artery disease (PAD) is narrowing of blood vessels around the body reducing circulation to body parts other than the brain or heart. PAD mainly affects blood vessels in the legs.
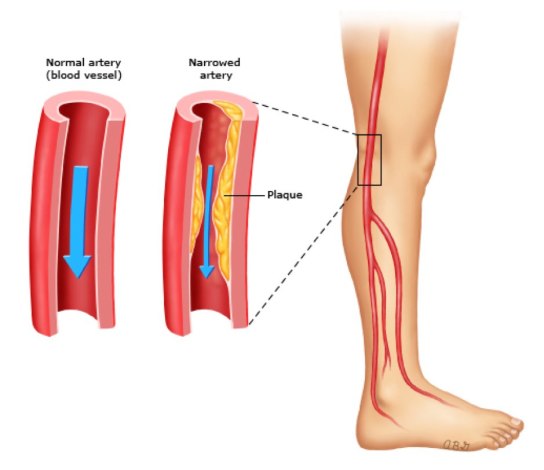
A symptom that you may have PAD is claudication. Claudication means “to limp” and is the development of deep pain in the leg muscles, including buttocks, thighs, and calves, and this can occur during activity. The pain in the legs goes away after resting.
Like cerebrovascular disease and coronary artery disease, PAD occurs as a result of atherosclerosis. The fatty plaque deposits block blood flow to the legs, including the muscles and skin.
What else do I need to know?
If you have diabetes, you will require ongoing check-ups to monitor for any diabetes-related complications. These routine examinations are important as early detection of any microvascular or macrovascular complications can lead to early interventions and treatment that may be able to reverse complications or prevent them from progressing further.
What should I do next?
If you experience any symptoms of type 1 diabetes or you have risk factors for developing type 1 diabetes, it is important to get tested for as soon as possible. Some people are at higher risk and need regular testing.
By diagnosing and treating the type 1 diabetes early, it means you can decrease the risk of developing or delay any further health complications of type 1 diabetes, for example nerve damage, blindness, and heart disease. It is important to know that diagnosing type 1 diabetes should not rely solely on using a Hb A1c test.
Once you learn what your type 1 diagnosis is, or if you already have type 1 diabetes, the next most important step is to become educated. You can join the 12-week Type 1 Diabetes Program to help you learn how best to manage the condition. For example, you can learn how best to monitor blood glucose levels in type 1 diabetes. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make. The first week is free and full of helpful and crucial information.
Interested in more information on type 1 diabetes?
Follow the links below to learn more about type 1 diabetes.
Frequently Asked Questions
What complications can occur with untreated type 1 diabetes?
Long-term high blood glucose damages blood vessels and increases the risk of both microvascular (eyes, kidneys, nerves) and macrovascular (heart, brain, legs) complications. Good glucose management, regular monitoring, and early treatment help reduce these risks.
What are the microvascular complications of type 1 diabetes?
Microvascular complications include diabetic retinopathy, diabetic nephropathy, and diabetic neuropathy. These conditions often develop silently, and the risk increases with the duration and level of hyperglycaemia. Early detection through regular screening is essential.
What is diabetic retinopathy?
Diabetic retinopathy is damage to the small blood vessels in the retina. It can cause vision loss or blindness. Because it may have no symptoms in early stages, routine eye examinations are crucial for early detection and treatment.
What is diabetic nephropathy?
Diabetic kidney disease occurs when long-term high glucose damages the kidney’s filtering system. Early signs include small amounts of albumin in the urine. It usually has no symptoms until advanced stages, so regular urine and blood tests are important.
What is diabetic neuropathy?
Diabetic neuropathy affects the nerves that control sensation, movement, and autonomic functions. Symptoms may include tingling, numbness, pain, or loss of protective sensation in the feet. Neuropathy increases the risk of foot ulcers and amputations, making regular foot care essential.
What are the macrovascular complications of type 1 diabetes?
Macrovascular complications include coronary artery disease, cerebrovascular disease (stroke), and peripheral artery disease. These conditions are linked to atherosclerosis. Managing glucose, blood pressure, cholesterol, and lifestyle factors reduces risk.
What is coronary artery disease in type 1 diabetes?
Coronary artery disease involves narrowing of the heart’s blood vessels, increasing the risk of heart attack. Warning symptoms include chest pressure or pain, discomfort in the arms, neck, jaw, back, or stomach, shortness of breath, nausea, sweating, palpitations, and dizziness. Seek emergency care if symptoms occur.
How does type 1 diabetes increase stroke risk?
Stroke occurs when blood flow to part of the brain is blocked or when a vessel ruptures. People with type 1 diabetes have a higher risk due to faster progression of atherosclerosis. Warning signs can be remembered by FAST: Face drooping, Arm weakness, Speech difficulty; Time to call emergency services.
What is peripheral artery disease in type 1 diabetes?
Peripheral artery disease is reduced blood flow to the legs caused by narrowed arteries. A typical symptom is calf, thigh, or buttock pain with walking that eases with rest (claudication). PAD increases the risk of ulcers and amputations, so regular foot checks and vascular risk reduction are essential.



