What is type 1 diabetes mellitus?
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — January 2026

What is Type 1 Diabetes?
Type 1 diabetes explained simply
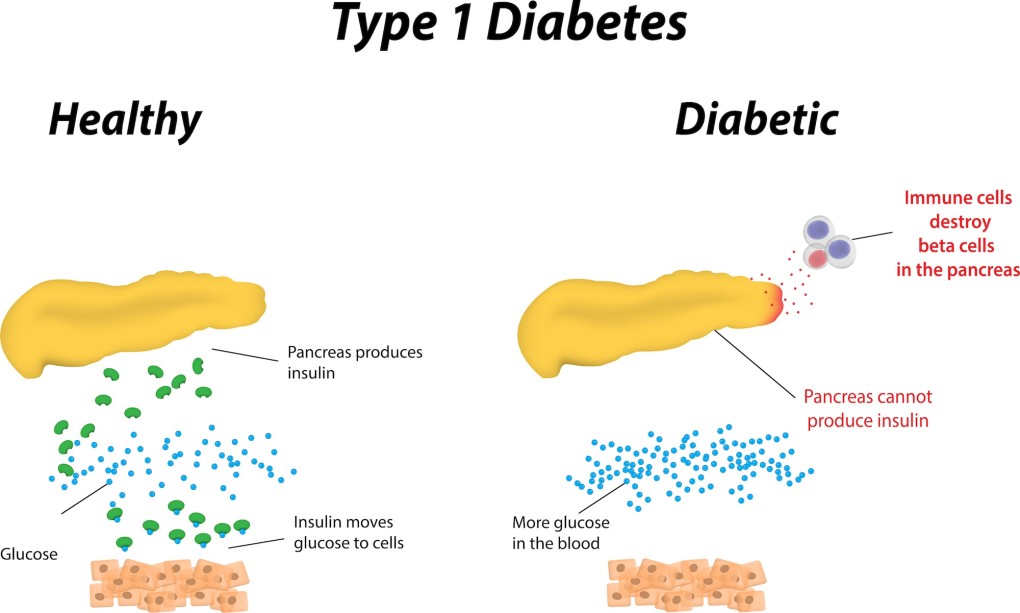
Type 1 diabetes causes high blood sugar levels because the body has little or no insulin.
In diabetes, glucose cannot enter the fat and muscle cells where it is needed for energy. To move glucose into a cell, the body needs a small molecule called insulin. This “key” unlocks the cell door. People with type 1 diabetes no longer produce enough insulin for a number of reasons.
Type 1 diabetes explained in more detail
Type 1 diabetes occurs when the pancreas—specifically the specialised cells within it called beta cells—fails to produce insulin. Most people with type 1 diabetes develop the condition when their immune system attacks and destroys these beta cells. This is why type 1 diabetes is called an autoimmune disease. The exact reason this happens is still being researched, but it’s likely that the immune system becomes confused and mistakes beta cells for a foreign invader such as a virus.
The fall in insulin production can happen quickly or slowly. Some people develop symptoms rapidly, over a few weeks or months, while others develop them more slowly over several years.
| Type 1 Diabetes Content |
|---|
| Type 1 Program |
| Overview |
| Risk Factors |
| Symptoms |
| Diagnosis |
| Complications |
| Treatment |
| Diet |
| Monitoring |
| Tools |
| Mental Health |
| Prevention |
Type 1 diabetes can also occur in someone who has had their pancreas removed. In this situation, a person can develop type 1 diabetes immediately after surgery. However, this is an uncommon cause.
Latent autoimmune diabetes in adults (LADA)
Latent autoimmune diabetes in adults, or LADA, is a form of type 1 diabetes that occurs later in life. “Latent” means that it develops slowly, so the signs and symptoms of LADA appear gradually compared to type 1 diabetes diagnosed in children. Because of this, LADA is sometimes mistakenly diagnosed as type 2 diabetes.
Some of the characteristics of LADA include:
- Onset at age 30 years or older
- Healthy body weight (BMI less than 25 kg/m²)
- Personal or family history of autoimmune disease
- Gradual onset of symptoms
Who is at risk of type 1 diabetes?
The simple answer is anyone. Although the risk increases if someone in your family has type 1 diabetes or another autoimmune condition such as coeliac disease, Addison’s disease, pernicious anaemia, or autoimmune thyroid disease. It can occur at any age, though it rarely develops in the first year of life. Even though it’s often associated with children, about half of all people who develop type 1 diabetes are over the age of 30.
What are the symptoms of type 1 diabetes?
The most common symptoms are thirst and frequent urination. These occur because high blood glucose levels cause glucose to pass into the urine, taking water with it. When blood glucose is very high, only a small amount can enter the muscle and fat cells. This leads to weight loss and loss of muscle mass. In the early stages, these symptoms may be mild and easy to miss.
You can read a full description of the symptoms of type 1 diabetes to learn more.
Type 1 diabetes and diabetic ketoacidosis
Diabetic ketoacidosis (DKA) happens when poisonous chemicals called ketones build up in the blood. DKA occurs in about 30% of children who present with type 1 diabetes (Diabetic Ketoacidosis in Infants, Children, and Adolescents). This causes the blood to become acidic, and the combination of acids and dehydration can lead to coma or even death.
DKA is a medical emergency that requires immediate treatment. Ketones often have a distinctive “nail polish remover” smell on the breath. Low levels of ketones can occur normally during prolonged fasting, with or without diabetes.
In a person with type 1 diabetes, the body cannot use glucose for energy. Instead, it uses stored fat, breaking it down for fuel. This breakdown releases ketones, which build up in the blood and appear in the urine.
Some symptoms of DKA include:
- Moderate to high ketones in the urine
- Rapid breathing
- Flushed cheeks
- Abdominal pain
- Sweet, acetone-like smell on the breath
- Vomiting
- Dehydration
How is type 1 diabetes diagnosed?
Several tests are used to diagnose type 1 diabetes, including fasting plasma glucose, random blood glucose, oral glucose tolerance test, and HbA1c. The first step is to confirm diabetes, followed by determining whether it is type 1 or another form.
Tests used to diagnose type 1 diabetes include:
- Fasting plasma glucose
- Random blood glucose
- Oral glucose tolerance test
- HbA1c test
Fasting plasma glucose
This test requires fasting for at least eight hours before a blood test. A fasting plasma glucose level above 7 mmol/L (126 mg/dL) on more than one occasion can indicate diabetes.
Random blood glucose
A random blood glucose test can be done at any time. A result of 11.0 mmol/L (200 mg/dL) or higher suggests hyperglycaemia (high blood glucose levels).
Oral glucose tolerance test
An oral glucose tolerance test (OGTT) involves drinking a glucose syrup followed by blood tests one and two hours later. A plasma glucose level of 11.0 mmol/L (200 mg/dL) or higher two hours after drinking the syrup can indicate diabetes. Most children and adolescents with type 1 diabetes already have very high blood glucose levels, so an OGTT is usually unnecessary for diagnosis.
Haemoglobin A1c (HbA1c) test
The HbA1c test measures how much glucose has attached to a type of haemoglobin—the oxygen-carrying molecule in our blood. It provides an estimate of average blood glucose control over two to three months. A reading of 6.5% or higher can indicate diabetes. However, some conditions can affect HbA1c accuracy. To learn more, visit the HbA1c test to diagnose diabetes article.
How this page fits into your learning
My Health Explained is designed to help you understand diabetes over time, not all at once. Most people arrive with one specific question, then build confidence as new questions come up.
This page covers one important part of that picture. You'll see links throughout to related topics that explain why things happen, what options exist, and what tends to help in real life.
If something here raises a question, follow the links that feel most relevant and ignore the rest for now. This resource is built to support learning at your own pace.
Want new articles and practical guides as we publish them? Subscribe to the newsletter.
Complications of untreated type 1 diabetes
Complications in type 1 diabetes are all related to poor blood glucose control. Poor control of blood glucose levels over a number of years can affect the blood vessels in the body, which can result in problems with the small blood vessels (known as microvascular complications) or the large blood vessels (known as macrovascular complications). The effects on the blood vessels from ongoing uncontrolled blood glucose levels, are a major source of morbidity and mortality for people with diabetes (Microvascular and Macrovascular Complications of Diabetes).
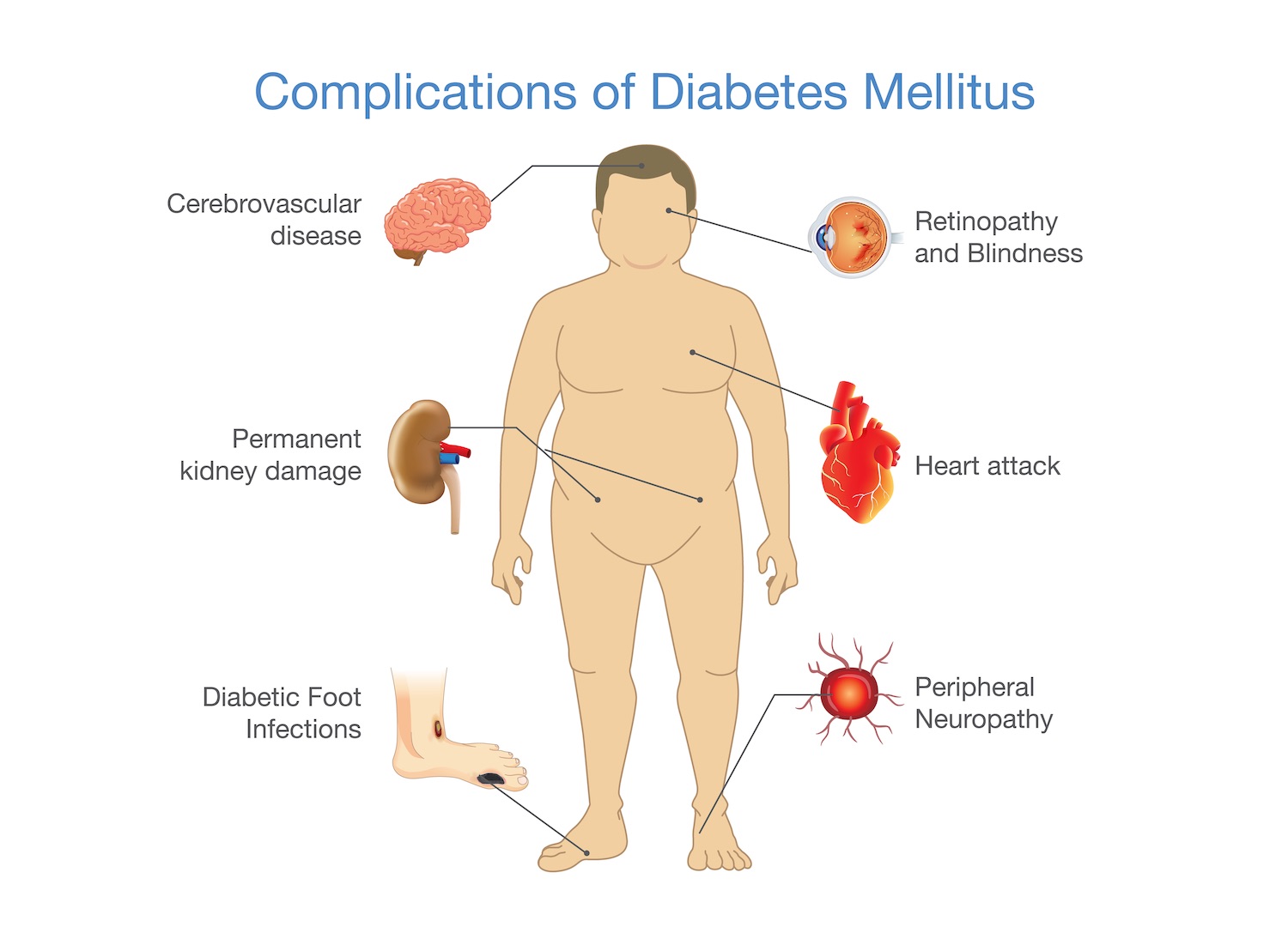
Microvascular complications – problems with small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 2 diabetes. Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Diabetic retinopathy is the most common microvascular complication of diabetes. In the U.K. Prospective Diabetes Study (UKPDS) it was found that most patients with type 1 diabetes, began to develop evidence of retinopathy within 20 years of diagnosis (Clinical Factors Associated With Resistance to Microvascular Complications in Diabetic Patients of Extreme Disease Duration).
Macrovascular complications - problems with large blood vessels
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- Coronary artery disease which can lead to a heart attack
- Cerebrovascular disease which can lead to a stroke
- Peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity as well as amputations.
Diabetes increases the risk of that a person will develop cardiovascular disease compared to someone who does not have diabetes. In fact, cardiovascular disease is the primary cause of death in people with type 1 diabetes (The effect of intensive diabetes treatment on resting heart rate in type 1 diabetes: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study).
To learn how to regain control of your blood glucose, you can join the 12-week personalised type 1 diabetes program. When you sign up, the first week is completely free!
How is type 1 diabetes treated?
In type 1 diabetes, treatment involves two key factors:
- Checking blood glucose levels regularly to make sure they aren’t too low or too high, and
- Using insulin (through a pen or pump) to help keep blood glucose levels in a safe range
Insulin is the main treatment for people with type 1 diabetes. The goal of insulin therapy is to replace insulin that can’t be produced by the pancreas to achieve normal glucose. Since insulin is a crucial hormone that allows glucose in the blood stream to get into the muscle and fat cells, replacing insulin is necessary for people with type 1 diabetes.
There are many different types of insulin and can be classified by the onset and duration of action. These include:
- rapid acting insulin
- intermediate acting insulin
- long acting insulin
Intensive insulin therapy can be delivered by either multiple daily injections (MDI) or through continuous insulin infusion (pump).
In the Diabetes Control and Complications Trial (DCCT), it was found that intensive therapy aimed at lower levels of blood glucose, resulted in decreased rates of retinopathy, neuropathy, and nephropathy in people with type 1 diabetes (The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus). The DCCT study also found that ongoing blood glucose control (for a period of 6.5 years) has the lasting benefit of reducing cardiovascular morbidity and mortality in people with type 1 diabetes.
Monitoring blood glucose levels in type 1 diabetes
Blood glucose levels can be monitored by self-monitoring or continuous glucose monitoring.
Self-monitoring of blood glucose levels
Self-monitoring is an integral part of type 1 diabetes therapy. It is necessary as it can indicate the amount of insulin that is required for correct dosing. Self-monitoring requires the use of a glucose meter.
Continuous glucose monitoring
Most continuous glucose monitoring devices transmit blood glucose levels every five minutes. They can even alert you if you’re experiencing a hypoglycaemic or hyperglycaemic event. Flash glucose monitoring is one type of continuous glucose monitoring.
What are the target blood glucose levels for type 1 diabetes?
Below are the target blood glucose levels for type 1 diabetes before meals and two hours after a meal.
Target blood glucose levels for Type 1 Diabetes Mellitus
| Target levels | mmol/L | mg/dL |
|---|---|---|
| Before meals | 4.0 - 8.0 mmol/L | 72 – 145 mg/dL |
| Two hours after starting meal | less than 10.0 mmo/L | less than 180 mg/dL |
Diet and exercise in type 1 diabetes
Diabetes education is essential to help someone better understand how diet and exercise can impact on type 1 diabetes. Carefully planning meal and activity times is essential, as eating raises blood glucose levels, while being active lowers it.
Nutrition
Carbohydrates play a crucial role in diabetes. Variations in carbohydrate intake can result in erratic blood glucose levels and hypoglycaemia. When first diagnosed with type 1 diabetes, it can take some time to get a handle on carbohydrates consistency. Some important aspects to consider when it comes to diet are:
- Estimating the amount of carbohydrate in food
- Carbohydrate counting
- Matching insulin to carbohydrate
- When to check blood glucose levels
Exercise
Regular physical activity and exercise is a significant component of diabetes management. Exercise has a number of benefits for all people and not just people with diabetes! The benefits of exercise include:
- Improved blood glucose control
- Weight control
- Reduction in the comorbidities hypertension, dyslipidaemia, and cardiovascular disease
- Improved mood
- Improved quality of life
While exercise has not consistently been shown to improve control for patients with type 1 diabetes, it is important to learn how to adjust diet or insulin to accommodate exercise and avoid hypoglycaemia. Other important considerations for type 1 diabetes and exercise include:
- Effect of exercise on blood glucose levels
- Late hypoglycaemia
- Type, intensity, and duration of exercise
- When to check blood glucose levels
- Types of snacks to have on hand to avoid hypoglycaemia
What should I do next?
If you experience any symptoms of type 1 diabetes or you have risk factors for developing type 1 diabetes, it is important to get tested for as soon as possible. Some people are at higher risk and need regular testing.
By diagnosing and treating the type 1 diabetes early, it means you can decrease the risk of developing or delay any further health complications of type 1 diabetes, for example nerve damage, blindness, and heart disease. It is important to know that diagnosing type 1 diabetes should not rely solely on using a Hb A1c test.
Once you learn what your type 1 diagnosis is, or if you already have type 1 diabetes, the next most important step is to become educated. You can join the 12-week Type 1 Diabetes Program to help you learn how best to manage the condition. For example, you can learn how best to monitor blood glucose levels in type 1 diabetes. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make. The first week is free and full of helpful and crucial information.
Find the Right Program for You
Select the situation that best describes you
Frequently Asked Questions
What is type 1 diabetes? (simple explanation)
Type 1 diabetes occurs when the body produces little or no insulin. Insulin acts like a key that allows glucose to move from the bloodstream into muscle and fat cells for energy. Without insulin, glucose builds up in the blood.
What is type 1 diabetes? (more detailed explanation)
Type 1 diabetes is an autoimmune condition where the immune system attacks and destroys the insulin-producing beta cells in the pancreas. The decline in insulin production can happen rapidly over weeks or more gradually over months.
What is LADA (latent autoimmune diabetes in adults)?
LADA is a slower-progressing form of autoimmune diabetes usually diagnosed in adults over 30. People may initially manage with tablets, but insulin is eventually required. Features can include normal or low BMI, a personal or family history of autoimmune disease, and gradual loss of insulin production.
Who is at risk of type 1 diabetes?
Anyone can develop type 1 diabetes at any age. Risk increases with a family history of type 1 diabetes or other autoimmune conditions such as coeliac disease, autoimmune thyroid disease, pernicious anaemia, or Addison’s disease.
What are the common symptoms of type 1 diabetes?
Typical symptoms include excessive thirst, frequent urination, tiredness, increased hunger, unintentional weight loss, and blurred vision. Symptoms may start suddenly or more gradually. Medical assessment is important if these occur.
What is diabetic ketoacidosis (DKA)?
DKA is a serious medical emergency caused by very low insulin levels, high ketones, and dehydration. Warning signs include rapid breathing, abdominal pain, vomiting, dehydration, confusion, and a fruity breath odour. Immediate treatment is essential.
How is type 1 diabetes diagnosed?
Diagnosis uses blood glucose tests and clinical assessment. Tests may include fasting glucose, random glucose, HbA1c, and sometimes an oral glucose tolerance test. Clinicians also consider age, symptoms, and autoantibody results to distinguish type 1 from other types.
What fasting plasma glucose indicates diabetes?
A fasting plasma glucose of 7.0 mmol/L (126 mg/dL) or higher on more than one occasion is consistent with diabetes.
What random plasma glucose indicates diabetes?
A random plasma glucose of 11.1 mmol/L (200 mg/dL) or higher with typical symptoms is consistent with diabetes.
What oral glucose tolerance test result indicates diabetes?
During a 75 g oral glucose tolerance test, a 2-hour glucose of 11.1 mmol/L (200 mg/dL) or higher indicates diabetes. In children and adolescents with symptoms, an OGTT is often unnecessary.
What HbA1c level indicates diabetes?
An HbA1c of 6.5% (48 mmol/mol) or higher can indicate diabetes, although some medical conditions affect HbA1c accuracy. Clinicians consider the full clinical picture.
What are complications of untreated type 1 diabetes?
Long-term high glucose increases the risk of retinopathy, kidney disease, nerve damage, heart disease, stroke, and peripheral artery disease. Good glucose, blood pressure, and cholesterol management reduce these risks.
How is type 1 diabetes treated?
Treatment requires insulin therapy (multiple daily injections or an insulin pump), regular glucose monitoring, education, nutrition support, and sick-day management to stay safe and maintain stability.
How are blood glucose levels monitored in type 1 diabetes?
Monitoring includes finger-prick glucose testing and continuous glucose monitoring (CGM). CGM devices provide frequent readings and alerts for high or low glucose, supporting safer day-to-day management.
What are common glucose targets in type 1 diabetes?
Targets vary by age and individual circumstances, but common goals include pre-meal levels of 4.0–8.0 mmol/L (72–145 mg/dL) and post-meal levels below 10.0 mmol/L (180 mg/dL), unless advised otherwise.
What nutrition factors are important in type 1 diabetes?
Carbohydrate estimation and carbohydrate counting are key skills. Matching insulin doses to carbohydrate intake, timing meals appropriately, and planning snacks around exercise help maintain stable glucose levels.
Why is exercise important in type 1 diabetes?
Exercise improves fitness, heart health, and emotional wellbeing. People with type 1 diabetes learn to balance insulin, food, and activity to reduce the risk of hypoglycaemia during and after exercise.



