What complications occur in type 2 diabetes? How likely is it that it will happen?
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — January 2026
Complications in type 2 diabetes
Type 2 diabetes is a complex condition, affecting many parts of your body. When people are diagnosed with type 2 diabetes mellitus, the disease process may have been present for 5-10 years. This means some complications may already be present at diagnosis.
When you have diabetes your blood sugars are elevated. Blood goes everywhere in your body so the effect of high sugars occur everywhere. A person with diabetes is at risk of many other health problems, including heart attacks, strokes, vision loss, nerve damage, and kidney disease. While this might sound overwhelming, there is some good news. You can take many steps to prevent any of these complications from occurring or becoming worse.
Statistics on the complications of type 2 diabetes
People with diabetes who have ongoing high blood glucose levels, are at an increased risk of having poor health outcomes compared to people who do not have diabetes. Some statistics that relate to people with diabetes include:
- People with diabetes are up to four time more likely to suffer heart attacks or strokes
- Diabetes is the leading cause of vision-loss globally and is the fifth most common cause of preventable blindness and fifth more common cause of moderate to severe visual impairment
- Kidney failure is three times more common in people with diabetes
- Amputations are 15 times more common in people with diabetes
- More than 30 percent of people with diabetes experience depression, anxiety, and distress
- Early diagnosis, optimal treatment, and effective ongoing support and management reduce risk of diabetes-related complications dramatically.
Let’s take a more in depth look into what can go wrong in someone who has diabetes.
Metabolic syndrome
Metabolic syndrome, sometimes called syndrome X, is a collection of disorders, including high blood pressure, insulin resistance, abnormal cholesterol levels, and excess fat around the waist. People with metabolic syndrome are twice as likely to have a heart attack and stroke, and five times more likely to develop type 2 diabetes, compared to people without metabolic syndrome.

Over the past three decades, the prevalence of Metabolic Syndrome has increased. Did you know that children and adolescents can also have metabolic syndrome? It’s not just adults! More and more young people are showing signs of metabolic syndrome. The incidence of metabolic syndrome often parallels the incidence of type 2 diabetes and obesity (The Global Epidemic of the Metabolic Syndrome). According to the Centers for Disease Control and Prevention (CDC), 12.2% or 30.2 million adults (aged 18 years and older) in the USA had type 2 diabetes in 2017. What’s scary, is that a quarter of these adults, don’t even realise that they have diabetes.
Typically, adults with type 2 diabetes will present with co-morbidities such as obesity, hypertension (high blood pressure), and dyslipidaemia (elevated cholesterol and fats in the blood). A co-morbidity is the presence of one or more additional diseases or disorders. Other co-morbidities that may be present at diagnosis or can develop over time, include gum disease, sleep apnoea, fatty liver disease, depression and anxiety, and bone fractures (Comprehensive Medical Evaluation and Assessment of Comorbidities by the American Diabetes Association).
If there are any complications present in a person with diabetes, the disease progression can be slowed by interventions, for example better management of blood glucose levels, blood pressure, and blood lipids.
What are the type 2 diabetes complications?
Diabetes is a vascular disease which means it affects blood vessels.
Complications in type 2 diabetes can be described as microvascular (small blood vessels) or macrovascular (large blood vessels) complications (Microvascular and Macrovascular Complications of Diabetes). As mentioned, diabetes-related complications occur over time due to persistent high blood glucose levels, high blood pressure, and abnormal cholesterol levels. These complications are serious and can be life-threatening.
Generally speaking, people with type 2 diabetes tend to experience macrovascular complications or cardiovascular complications mainly but they can still experience microvascular complications too.
Macrovascular complications - Problems with large blood vessels
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- coronary artery disease which can lead to a heart attack called cardiovascular disease.
- cerebrovascular disease which can lead to a stroke or cerebrovascular disease.
- peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity as well as amputations. This is referred to as peripheral vascular disease.
Studies have shown that in people with type 2 diabetes, poor blood glucose control increases the risk of macrovascular complications (Glycaemic control and vascular complications in type 2 diabetes mellitus). Studies have also shown that by treating and controlling hypertension and dyslipidemia, can aid in reducing the risk of macrovascular disease.
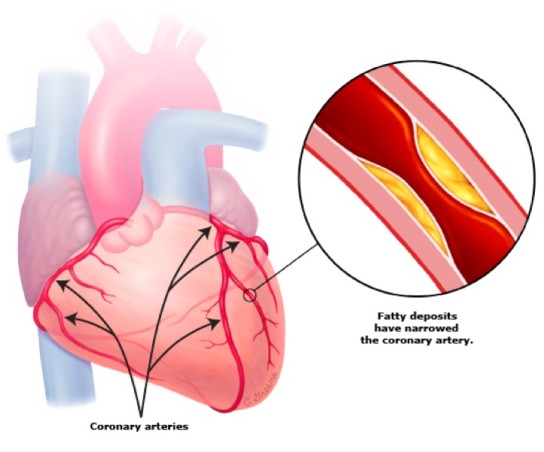
The main cause for these macrovascular diseases is atherosclerosis (Diabetes and atherosclerosis: epidemiology, pathophysiology, and management). Atherosclerosis is a build-up of fatty deposits in the blood vessels, typically the arteries. These fatty plaques can grow over time and result in narrowing of the blood vessels or completely blocking blood flow.
Atherosclerosis can occur anywhere in the body. When it occurs in the arteries of the heart, it is called coronary artery disease. When it occurs in the arteries of the brain, it is called cerebrovascular disease. Finally, when atherosclerosis occurs in the arteries supplying blood to other areas of the body like the legs or kidneys, it is called peripheral artery disease.
Coronary artery disease
Coronary artery disease is a condition that puts you at risk of a heart attack and other forms of heart disease. The coronary arteries supply blood to the heart muscles and when these arteries become narrow due to atherosclerosis, it can lead to a heart attack. Cardiovascular disease is actually the number one killer of people with type 1 or type 2 diabetes (Microvascular and Macrovascular Complications of Diabetes).
Typically, the first sign that someone has heart disease, and even diabetes, is when they have a heart attack called a myocardial infarction or MI (myo meaning muscle, cardial meaning heart). Some people who have heart disease may experience chest pain even if they aren’t having a heart attack or myocardial infarction. This can happen while they are walking, going up stairs, or just moving around.
It is important to be able to recognise the symptoms of a heart attack. They can include:
- Pain, pressure or discomfort in the centre of the chest
- Pain, tingling or discomfort in other parts of the upper body including the arms, back, neck, jaw, and stomach
- Shortness of breath
- Nausea, vomiting, heartburn, or burping
- Sweating or having cold, clammy skin
- Racing or uneven heartbeat
- Feeling of dizziness or light-headedness
If you experience any of these symptoms for more than 10 minutes, or they keep coming or going, or any pain in your chest you experience is new or different, contact your emergency services for an ambulance right away.
Stroke (cerebrovascular disease)
Cerebrovascular refers to blood flow to the brain. Cerebrovascular disease refers to all disorders whereby the brain is temporarily or permanently affected by inadequate blood flow or bleeding in one or more of the blood vessels to the brain. This may occur due to a stroke. There are 2 main types of stroke, ischaemia where a blood vessel becomes blocked due to a narrowing or clot. This is called infarction.
The second type of stroke is when a blood vessels bursts and bleeds into the brain, termed haemorraghic stroke. In both types of stroke the brain tissue downstream from the blood vessel is starved of oxygen and starts to deteriorate and die very quickly.
One way that blood flow can be restricted to the brain is through narrowing of the blood vessels, for example in the carotid arteries. Blockages in these arteries, severely increases a person’s risk of having a stroke. A stroke is when a part of the brain becomes damaged due to problems with blood flow in the brain.
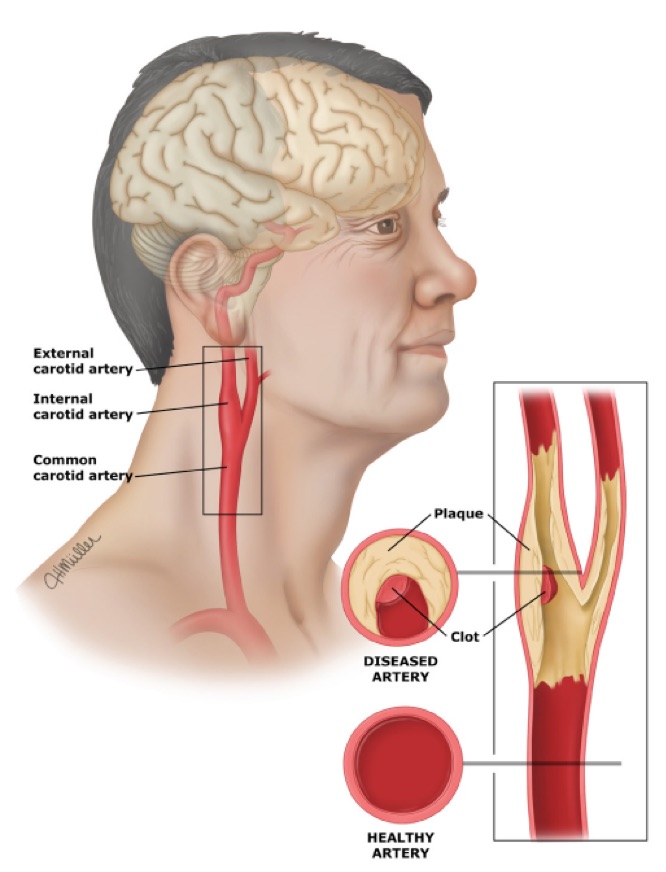
Blood clots or the fatty plaque deposits can break off and travel to smaller blood vessels in the brain, where it can cause a blockage and lead to a stroke. A stroke may also occur when an artery breaks open causing excessive bleeding into and around the brain.
The lasting effects of the stroke can differ for everyone and can also depend on how quickly you receive treatment and which part of your brain is affected. For some people who have had a stroke, they may recover with only minor problems, but many people have ongoing issues. Following a stroke, some people may be:
- Unable to understand speech or are unable to speak themselves
- Paralysed down one side of the body, including the side of the face, the arm, and the leg
- Unable to take care of themselves, including to dress and feed themselves
If you are unsure of the warning signs of when someone is having a stroke, think of the word “FAST.” Each letter stands for signs to look out for:
- Face – Does the face look uneven or droop on one side?
- Arm – Does the person have weakness or numbness in one or both arms?
- Speech – Is the person having trouble speaking? Does the speech sound strange?
- Time – If you notice any of these signs, it’s time to call the ambulance.
Peripheral artery disease
Peripheral artery disease (PAD) is narrowing of blood vessels around the body reducing circulation to body parts other than the brain or heart. PAD mainly affects blood vessels in the legs.
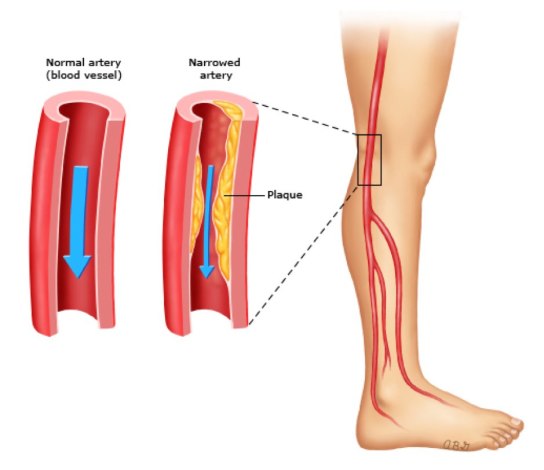
A symptom that you may have PAD is claudication. Claudication means “to limp” and is the development of deep pain in the leg muscles, including buttocks, thighs, and calves, and this can occur during activity. The pain in the legs goes away after resting.
Like cerebrovascular disease and coronary artery disease, PAD occurs as a result of atherosclerosis. The fatty plaque deposits block blood flow to the legs, including the muscles and skin.
Microvascular complications - problems with small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 2 diabetes.
Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Retinopathy, nephropathy, and neuropathy are all progressive disorders. These complications won’t be noticeable at the beginning as they don’t produce any symptoms during the early stages. They can also be prevented, or the severity minimized with the combination of regular medical check-ups and adequate blood glucose management. Similar to macrovascular complications, microvascular complications can increase with ongoing poor blood glucose control as well as the duration that you have had diabetes. This means, the longer that you have had diabetes and the longer you have had high blood glucose levels, means that you are more likely to develop diabetes-related complications. So! The earlier that any of these complications are detected, means that early intervention can occur which may be able to reverse any of these microvascular diseases or help to delay further progression.

Looking for more diabetes videos?
Check out our latest diabetes videos for more great content.
How this page fits into your learning
My Health Explained is designed to help you understand diabetes over time, not all at once. Most people arrive with one specific question, then build confidence as new questions come up.
This page covers one important part of that picture. You'll see links throughout to related topics that explain why things happen, what options exist, and what tends to help in real life.
If you'd like a broader overview first, start here: What is type 2 diabetes mellitus?.
If something here raises a question, follow the links that feel most relevant and ignore the rest for now. This resource is built to support learning at your own pace.
Want new articles and practical guides as we publish them? Subscribe to the newsletter.
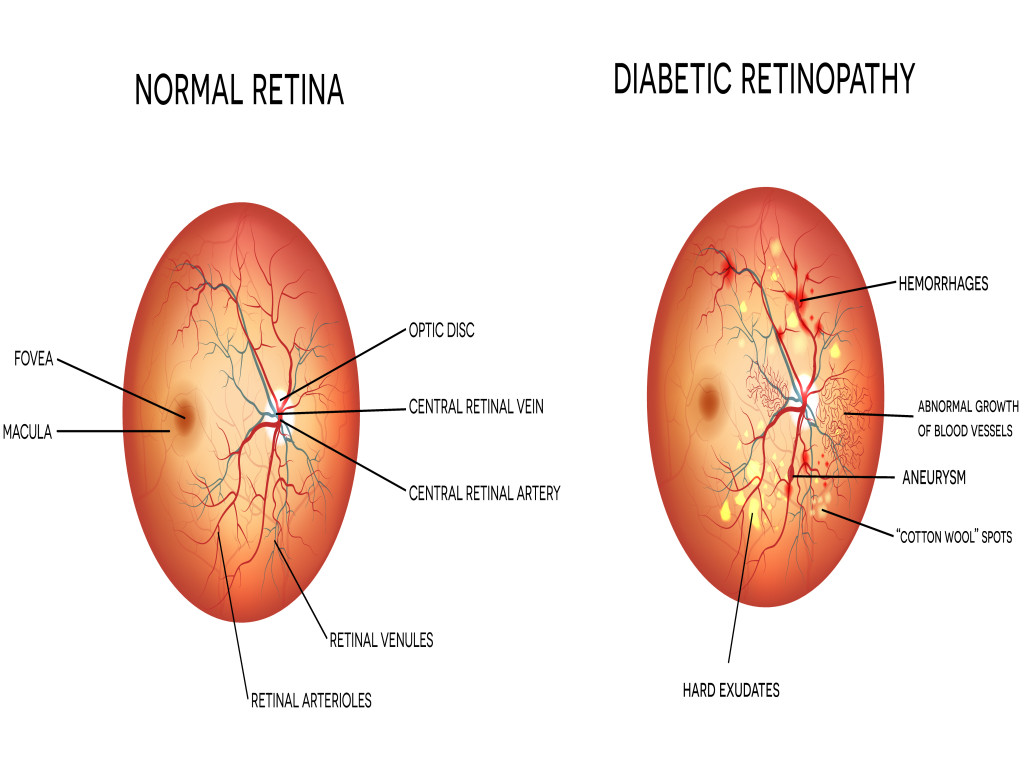
Retinopathy
Eye problems in people with diabetes, is known as diabetic retinopathy. It can lead to loss of vision and even blindness (Diabetic Retinopathy). Retinopathy affects the small blood vessels of the retina at the back of the eye. For most people, retinopathy will have no symptoms until the disease is quite advanced. Unfortunately, by then there is little that can be done about any vision loss. This is why early detection is so important.
There are three stages of retinopathy. Most people who have type 2 diabetes develop the mildest form (nonproliferative retinopathy). For some people, this can progress to the intermediate stage of retinopathy (pre-proliferative retinopathy), or even to the advanced stage of retinopathy (proliferative retinopathy) which carries the highest risk of blindness.
Nephropathy
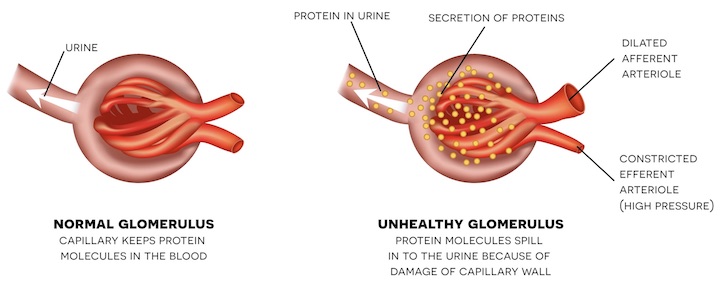
Did you know that in the United States, diabetic nephropathy is the leading cause of kidney failure? (Microvascular and Macrovascular Complications of Diabetes). Diabetes-related nephropathy affects the small blood vessels in the kidney, which can alter the normal function of the kidney. The kidneys are responsible for filtering our blood and removing any waste products and excess salts and water from our blood. When the kidneys are functioning normally, they prevent protein leaking into our urine. So, if there is protein found in the urine, this is often the first sign of nephropathy.
If you have diabetes, you may not even realise that you have any problems with your kidneys. You may still even be producing normal amounts of urine. But did you know that people with diabetic kidney disease usually don’t exhibit any symptoms until at least 75 percent of the kidneys’ function is lost! (Diabetic Nephropathy: Diagnosis, Prevention, and Treatment.)
Neuropathy
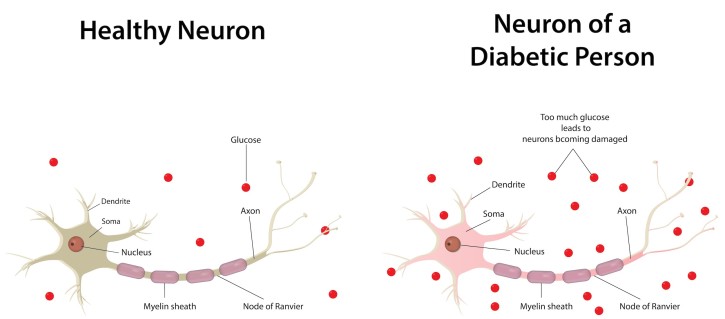
Diabetes-related neuropathy is also a progressive disorder affecting our nerves. Nerves have important roles in our body, as they act to transmit signals all over our body. Our nervous system has a wide range of jobs including, controlling our heart rate and blood pressure, as well being responsible for nerve conduction and sensory perception.
Did you know that 10-18% of adults with type 2 diabetes show signs of nerve damage by the time they’re diagnosed with diabetes? As discussed in symptoms of type 2 diabetes, the most common sign of diabetes is nothing at all. It can sometimes take 5-10 years before someone is diagnosed with diabetes, and by that point they may already have symptoms of reduced nerve function.
Diabetic neuropathy can lead to amputations in some people with diabetes. It has been found to be responsible for more than 80% of amputations that occur after a foot injury or foot ulcer, which can result from diabetic neuropathy (The Association Between Cardiovascular Autonomic Neuropathy and Mortality in Individuals with Diabetes).
What else do I need to know?
If you have diabetes, you will require ongoing check-ups to monitor for any diabetes-related complications. Monitoring your diabetes is essential. These routine examinations are important as early detection of any microvascular or macrovascular complications can lead to early interventions and treatment that may be able to reverse complications or prevent them from progressing further.
Eye exams
Routine eye exams help to monitor changes in the blood vessels in the eye. They’re important as diabetic-related retinopathy may lead to blindness in some people who have type 2 diabetes.
When examining your eyes, your doctor may perform one of the following tests:
- Dilated eye exam - Your doctor will use special eye drops that help to open up your pupils, allowing them to examine the retina at the back of the eye.
- Digital retinal imaging - Using a special camera, a technician will take pictures of the back of your eye, before sending the images to a specialist eye doctor.
If you have type 2 diabetes, you should have your eyes checked regularly as soon as you are diagnosed with diabetes. If you already have retinopathy, you will need to get your eyes checked at least once a year, possibly more, however your doctor will decide what the best schedule for you is.

Foot exams
Foot problems are a common occurrence in people with diabetes. With proper care, these foot complications can be prevented, so if you have diabetes, your feet need to be visually inspected whenever you see your doctor. These visual inspections can help to identify any problems with your toenails, fungal infections, or ulcers caused by poorly fitting shoes. As well as regular foot examinations, a comprehensive foot exam should be performed annually to identify any risk factors that could lead to ulcers and amputation.
When your doctor or healthcare provider checks your feet, they will check for the following:
- Poor circulation
- Nerve damage
- Skin changes
- Deformities
- Foot reflexes
- Sensory perception
It is important that you inform your doctor of any changes that you may have noticed with your feet.
You can also conduct foot exams at home. Self-care is essential when it comes to foot care, and in this instance, the patient becomes a vital member of the healthcare team!

Can I prevent type 2 diabetes?
You may have just found out that you are at risk of developing diabetes. This may be more difficult than you anticipated. However, if you don’t have diabetes yet, this is actually really good news. It means that you can make changes now to prevent or delay developing type 2 diabetes. Making some simple changes now, can have a huge impact on your health for the years ahead.
So, yes! You can prevent type 2 diabetes. Phew!
What can I do to prevent type 2 diabetes?
There are changes you can make to improve your health and reduce your risk of developing diabetes. These include:
- Eating well
- Moving your body more
- Being a healthy weight
- Setting realistic goals
- Getting support
- Make changes part of your everyday
There is also some evidence that suggests quitting smoking can help to reduce your risk of developing diabetes. While there still needs to be more research done in this by scientists, there are plenty of other great reasons to quit smoking. For example, quitting smoking can help to lower your risk of having a stroke or heart attack.
Making these changes can also help to reduce your risk of developing diabetes comorbidities; hypertension and dyslipidemia.

Interested in more information on type 2 diabetes?
Follow the links below to learn more about type 2 diabetes.
Frequently Asked Questions
What complications can occur with type 2 diabetes?
Type 2 diabetes can damage blood vessels and nerves over time. Complications are usually grouped into macrovascular complications (affecting the heart, brain, and legs) and microvascular complications (affecting the eyes, kidneys, and nerves). The risk of these diabetes complications rises with long-term high blood glucose levels, high blood pressure, and abnormal cholesterol or triglycerides.
What are macrovascular complications in type 2 diabetes?
Macrovascular complications in type 2 diabetes involve the larger blood vessels. They include coronary artery disease (which can lead to heart attacks), cerebrovascular disease (which can lead to stroke), and peripheral artery disease in the legs (which can cause pain on walking, poor circulation, ulcers, and increase the risk of amputation).
What are the warning signs of a heart attack?
Warning signs of a heart attack can include chest pain, pressure, tightness, or discomfort; pain, tingling, or discomfort in the arms, back, neck, jaw, or stomach; shortness of breath; nausea, vomiting, or heartburn; sweating or cold, clammy skin; a fast or irregular heartbeat; and dizziness or light-headedness. If any of these symptoms last more than a few minutes or keep coming and going, call emergency services immediately.
How are strokes linked to diabetes?
Type 2 diabetes accelerates atherosclerosis (fatty build-up in the arteries), which increases the risk of stroke. Narrowed or blocked blood vessels in the brain can cause an ischaemic stroke, while fragile vessels are more prone to bleeding, causing a haemorrhagic stroke. In both cases, reduced blood flow deprives brain tissue of oxygen and can lead to sudden, permanent injury if not treated urgently.
What are the stroke warning signs (FAST)?
The FAST signs help you remember stroke symptoms: Face – one side of the face may droop or feel numb; Arm – weakness, numbness, or inability to lift one arm; Speech – slurred speech, difficulty speaking, or trouble understanding others; Time – if you notice any of these signs, call emergency services immediately. Fast treatment can reduce brain damage and improve recovery.
Does diabetes increase the risk of amputations?
Yes. Diabetes increases the risk of amputations, especially of the toes, feet, and legs. Peripheral artery disease reduces blood flow, and diabetic neuropathy can reduce feeling in the feet. Together with a higher risk of infection, this makes ulcers slower to heal and more likely to become severe. Claudication – aching or cramping pain in the legs during walking that improves with rest – can be an early warning sign of poor circulation.
What are microvascular complications in type 2 diabetes?
Microvascular complications affect the small blood vessels and include diabetic retinopathy (eye disease), diabetic nephropathy (kidney disease), and diabetic neuropathy (nerve damage). These changes often begin silently, with no symptoms at first, and gradually worsen if blood glucose, blood pressure, and cholesterol remain high over many years.
What is diabetic retinopathy?
Diabetic retinopathy is damage to the tiny blood vessels in the retina, the light-sensitive tissue at the back of the eye. Leaking or blocked vessels can cause blurred vision, floaters, visual field loss, and, in advanced stages, blindness. Because early diabetic eye disease may have no symptoms, regular dilated eye examinations are essential for people with type 2 diabetes to detect problems early and allow timely treatment.
What is diabetic nephropathy?
Diabetic nephropathy is kidney damage caused by long-term high blood glucose and high blood pressure. Early on, protein starts to leak into the urine, which can be detected on urine tests even when you feel well. Over time, kidney function can gradually decline, potentially leading to chronic kidney disease and, in severe cases, kidney failure. Regular blood and urine tests help pick up diabetic kidney disease early so treatment can slow its progression.
What is diabetic neuropathy?
Diabetic neuropathy is nerve damage related to diabetes. It can affect sensation, pain, and autonomic functions such as heart rate, blood pressure, and digestion. In the feet and legs, reduced feeling, burning, tingling, or numbness increase the risk of unnoticed injuries, ulcers, and infection. Many people already have some degree of neuropathy when type 2 diabetes is diagnosed, making routine foot checks, good footwear, and regular podiatry care very important.







