There is a correlation between high Hb A1c levels and diabetes-related complications. Reducing your Hb A1c can reduce your risk of developing complications in type 2 diabetes.
Medically reviewed by Dr Sultan Linjawi, Endocrinologist & Diabetes Specialist — January 2026
Type 2 diabetes mellitus is a leading cause of preventable morbidity and mortality. Type 2 diabetes is associated with a number of microvascular and macrovascular complications. If you have type 2 diabetes, good blood glucose control is essential in preventing or delaying diabetic complications.
Hb A1c can be a useful measure of blood glucose control and can be used as a means to assess chronic high blood glucose levels. Through a number of studies, high Hb A1c readings have been found to be associated with the risk of long-term diabetes-related complications.
The prevalence of type 2 diabetes
It’s no secret how devastating the effect of diabetes is worldwide. Globally, diabetes is a major contributor to early illness and death. The World Health Organisation estimated that diabetes was the seventh leading cause of death in 2016, with diabetes being a direct cause of 1.6 million deaths worldwide (Diabetes).
What is the HbA1c test?
The HbA1c test, or the glycated haemoglobin A1c test, is a blood test that can be taken at any time as you don’t need to fast before taking the test. It indicates what your average blood glucose levels are over the past three months, by measuring the percentage of blood glucose that has attached to haemoglobin. Haemoglobin is the oxygen carrying protein found in red blood cells.
What is haemoglobin?
Haemoglobin is the iron-containing protein that is responsible for transporting oxygen in red blood cells. It helps to carry oxygen from our lungs to the rest of the body.
What do the different HbA1c readings mean?
It is normal for all people to have some glucose attached to haemoglobin. In people with diabetes, the higher the blood glucose levels are, the more glucose you have attached to haemoglobin.
A healthy person, without diabetes, has a HbA1c level below 5.7%
Someone with prediabetes (sometimes called borderline diabetes), has a HbA1c level between 5.7 and 6.4%
In people with diabetes, a HbA1c level of 6.5% or higher, from two separate tests, can indicate diabetes.
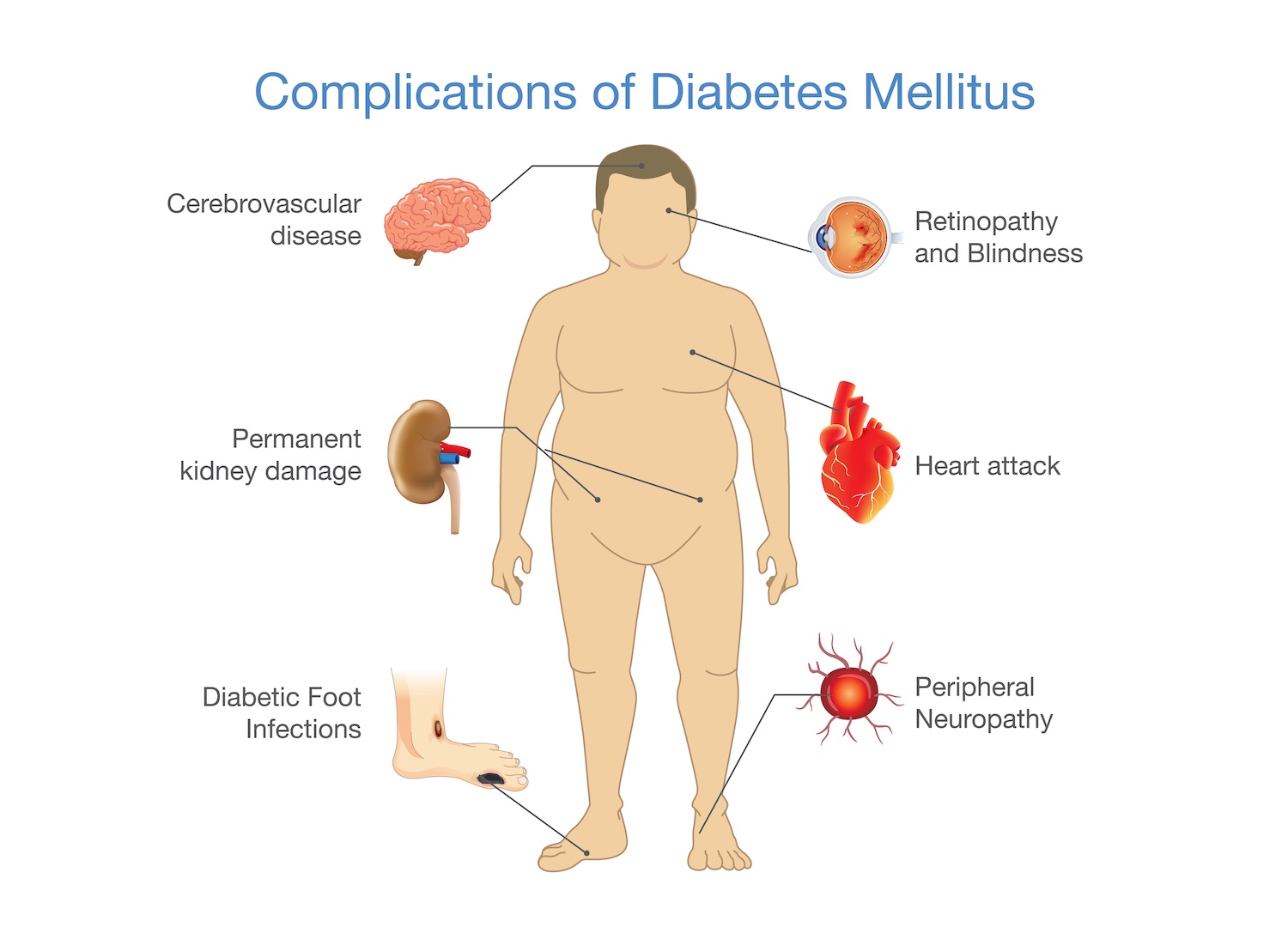
What are the complications of type 2 diabetes?
It is well known that diabetes is a complex condition, affecting many parts of your body. When people are diagnosed with type 2 diabetes mellitus, the disease process has often been present for 5-10 years, which means some complications may already be present at time.
When you have diabetes, you are at risk of many other health problems, including heart attacks, strokes, vision loss, nerve damage, and kidney disease. While this might sound overwhelming, there is some good news. You can take many steps to prevent any of these complications from occurring or becoming worse.
Diabetes is a vascular disease and complications in type 2 diabetes can be described as microvascular (small blood vessels) or macrovascular (large blood vessels) complications (Microvascular and Macrovascular Complications of Diabetes).
As mentioned, diabetes-related complications occur over time due to persistent high blood glucose levels, high blood pressure, and abnormal cholesterol levels. These complications are serious and can be life-threatening.
Macrovascular complications – problems with the large blood vessel
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- coronary artery disease which can lead to a heart attack
- cerebrovascular disease which can lead to a stroke
- peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity.
Studies have shown that in people with type 2 diabetes, poor blood glucose control increases the risk of macrovascular complications (Glycaemic control and vascular complications in type 2 diabetes mellitus). Studies have also shown that by treating and controlling hypertension and dyslipidemia, can aid in reducing the risk of macrovascular disease.
Microvascular complications – problems with the small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 2 diabetes.
Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – disease of the kidneys which can lead to kidney failure and the need for dialysis
Retinopathy, nephropathy, and neuropathy are all progressive disorders. These complications won’t be noticeable at the beginning as they don’t produce any symptoms during the early stages. They can also be prevented, or the severity minimized with the combination of regular medical check-ups and adequate blood glucose management. Similar to macrovascular complications, microvascular complications can increase with ongoing poor blood glucose control as well as the duration that you have had diabetes. This means, the longer that you have had diabetes and the longer you have had high blood glucose levels, means that you are more likely to develop diabetes-related complications. So! The earlier that any of these complications are detected, means that early intervention can occur which may be able to reverse any of these microvascular diseases or help to delay further progression.
You can read more about what can go wrong in diabetes and how likely it will happen to you, in our article about the (microvascular and macrovascular complications of type 2 diabetes.
Hb A1c and the association with long-term complications
Good blood glucose control can reduce the risk of developing microvascular and macrovascular complications associated with type 2 diabetes mellitus. It can also delay the progression of diabetes complications.
Hb A1c readings can indicate glycaemic control from the previous 3 months in people with diabetes. People who have diabetes have higher levels of HbA1c, which could be two to three times higher than normal. There is a strong relationship between high Hb A1c readings and the risk of developing diabetes-related complications, including cardiovascular disease, retinopathy, and neuropathy. So good blood glucose control is essential to prevent diabetic complications.
A number clinical trials have demonstrated that intensive therapy aimed at reducing blood glucose levels, results in decreased rates of microvascular complications (retinopathy, neuropathy, and nephropathy). Every 1 percent decrease in Hb A1c is associated with improved outcomes for people with diabetes. However, the benefits of reducing Hb A1c must be weighed against the risk of severe hypoglycaemia, especially for people with type 2 diabetes.
UKPDS
The United Kingdom Prospective Diabetes Study (UKPDS) investigated the role of glycaemic control in patients with newly diagnosed type 2 diabetes mellitus, using intensive treatment and conventional treatment. Intensive treatment involved medications to control blood glucose levels, whereas the conventional treatment involved diet to control blood glucose levels.
Participants in one of the study groups, took metformin as a treatment for glycaemic control, and compared the results to the conventional, diet therapy. The study went on to show the benefits of metformin, where metformin use compared to diet therapy, resulted in a risk reduction of 32% for both macrovascular and microvascular complications in overweight diabetic patients (Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group.). Metformin was also demonstrated to reduce diabetes-related death by 42%. When compared to the other medication study group (using sulfonylurea or insulin), metformin had a greater impact on the reducing complications compared to sulfonylurea or insulin. We’ve also written an article about the benefits of metformin.
Throughout the duration of the follow-up period (over approximately 17 years), it was found that intensive treatment in glycaemic control, produces better long-term outcomes, including fewer overall deaths, fewer diabetes-related deaths, and fewer heart attacks, when compared to conventional treatment.
How can I lower by Hb A1c and reduce my risk of developing complications of type 2 diabetes?
If you have diabetes, you can improve and lower your Hb A1c readings and reduce your risk of developing diabetic complications. You can lower your Hb A1c through:
- Improving your diet
- Exercising and moving your body more
- Taking your medications as prescribed
- Checking your blood glucose levels regularly
Diet
Making the right changes in your diet can help you to reduce your Hb A1c levels. You can do this by:
- Reducing your portion sizes
- Reducing your intake of discretionary items and processed foods
- Choosing water as your primary beverage
Reduce your portion sizes
You probably realise that eating more food = more calories and energy. Reducing your portion sizes means that you’ll be eating less food (duh) which can help you to lose weight. The majority of people eat meals that are way too large. This increasing excessive energy consumption, coupled with low physical activity, can result in weight gain and diabetes.
You might think, “but I’ll go hungry if I reduce my portion sizes too much!” I promise you, you will not go hungry. Yes, it can be hard to make some changes to your portion sizes, but here are some tips of what you can do:
- Serve less – when serving your meal, put slightly less food on your plate than you normally would
- Use a smaller a plate – if you’re eating off of a smaller plate, your meals will look like it fills up more of the plate, so you won’t feel as though you’re necessarily missing out
- Make less – when preparing your meals, make less so you are less likely to add more food to your plate, or else portion out the excess into reusable containers for easy lunch options for the week ahead
- Avoid distractions while eating – if you can, sit and enjoy a meal with your friends or family as eating in front of a TV causes us to eat more!
Some studies have found the benefits of portion control in people with prediabetes. One study ( Body composition, dietary composition, and components of metabolic syndrome in overweight and obese adults after a 12-week trial on dietary treatments focused on portion control, energy density, or glycemic index) found that portion control as a weight loss method resulted in lower blood glucose and insulin levels in participants after a 12-week period. Another study of men with prediabetes (Improvement in diet habits, independent of physical activity helps to reduce incident diabetes among prediabetic Asian Indian men), found that in combination with other healthful behaviours, those who reduced their portion sizes lowered their risk of developing diabetes compared to men who made no lifestyle changes at all. Lowering your blood glucose levels means lowering you Hb A1c levels.
Reducing your intake of discretionary items and processed foods
Discretionary items are often referred to as ‘sometimes foods’ or ‘junk food’! Cakes, biscuits, lollies, and other sweet foods are well known as being ‘sometimes foods.’ Did you know that processed foods, including bacon, meat pies, and deli meat are also considered discretionary items? These types of foods are typically high in sugar, fat, and salt. These foods, especially the ones that are high in sugar, can impact on both your blood glucose levels, as well as your weight.
It’s also important to note that these types of foods also contribute to developing and worsening of comorbidities of diabetes, for example hypertension and high cholesterol.
Choosing water as your primary beverage
When it comes to hydration, having a glass of water is the best option. Here are two great things about water: it’s free from our taps and it’s free from energy. If you are someone who drinks a lot of juice or soft drink (including soda water), you might not realise how much extra energy you are consuming and what impact it is having on your blood glucose levels.
For example, a small glass or 125mL of fruit juice may equal 255kJ or 60 calories. But we have so many different sized cups and glasses at home, often opting for larger glasses. If you were to have a bigger glass of juice, for example a cup or 250mL, and you had 2 or 3 of these a day, you could be having an extra 1020kJ (242 calories) to 1530kJ (363 calories). And that’s on top of any meals or snacks you are having! It can all add up really quickly.
Reducing drinks like fruit juice or soft drinks from your diet, not only saves you money and assists in your weight loss, it may also decrease your blood glucose and insulin levels.
On the topic of fruit juice, here is a quick little video about fruit juice: Should I drink fruit juice?
For more information about diet and diabetes, read these articles:
- Carbohydrates and Diabetes
- How to reduce carbs in your diet
- Yo-Yo Dieting – More serious than just gaining weight
Exercise
Exercise doesn’t have to be going to the gym at 5am or doing crossfit seven days a week. Exercise means something different to everyone. The important thing is that we do something! Avoiding sedentary behaviours and moving more can help to prevent diabetes, hypertension, and dyslipidemia. It can also reduce your blood glucose levels.
When it comes to exercising, it is important for you to choose activities that you enjoy as it makes moving your body far more exciting. Maybe you have a bike in the shed that is gathering a bit of dust, but you miss the feel of the wind blowing through your hair. Maybe you miss swimming when it’s really hot. Or maybe you’ve always wanted to take up salsa dancing. Whatever it is, finding an activity you like that can fit into your daily routine, will mean that you’re more likely to stick with it for the long haul.
If it has been a little while since you’ve last exercised, starting off with a morning or afternoon walk might be more suitable for you. Walking is a great way to slowly introduce exercise back into your life. You can start by walking around the block and increase the distance of your walk little by little every day.
Some other ways to move your body more, especially if you work an office job, can include going for a walk on your lunch break or even walking to the sink to fill up your water glass every hour. If you often have meetings with your co-workers, try to go on a walking meeting, even if it’s just around a block. It’s also a great way to get some fresh air and have time out from staring at your computer screen.
Ideally when we exercise, we should be aiming for at least 30 minutes or more of aerobic exercise on most days of the week. You could even break it up into three lots of 10 minutes and spread it across the day! Remember, if it’s been awhile since you were last active, start slowly and build gradually. Maybe you could even give Exercise Snacking a go!
Once you start to move your body more and become more used to exercising, it becomes easier and easier, and the benefits keep rolling in!! You will become fitter and lose more weight. With your increased fitness and less body weight to move, you will be able to exercise even more and push yourself to reach any new exercise goals you have.
For more information about exercise and diabetes, read these articles:
- 4 easy diet and exercise steps!
- Exercise snacking – An easy way to achieve weight loss and improve diabetes
- Is sitting making us sick?
Medication
If your doctor has given you medication, it is important that you take the medication as prescribed. Following your treatment plan given to you by your doctor is essential. The medications will help to reduce your blood glucose levels and Hb A1c levels, in combination with diet and exercise of course! Don’t forget that they’ll only work when you take them regularly.
For more information on some common diabetes medications, read the following articles and watch the videos:
- Benefits of Metformin: a wonder drug?
- Trulicity (Dulaglutide) – How do I use it and what does it do?
- What is Ryzogen insulin and how do I use it?
Monitoring
Checking your blood glucose levels (BGL) regularly is an important part of diabetes management. You blood glucose readings reflects how your diet, exercise, and medications have been impacting on your BGLs.
Don’t forget to check your blood glucose levels before and after food, exercise, and other activities. By monitoring your BGLs regularly, you’ll be able to better understand how your diet and exercise is impacting on your readings. You might realise that something you’re doing isn’t working for you, and your BGLs are still quite high. You’ll be able to take any necessary steps to keep your BGLs under control.
To the point
- High Hb A1c readings have been found to be associated with the risk of long-term diabetes-related complications
- Lowering Hb A1c readings can reduce your risk of developing complications
- Complications of type 2 diabetes include problems with the small blood vessels (retinopathy, neuropathy, nephropathy) and the large blood vessels (stroke, peripheral artery disease, and heart attack)
- You can reduce your Hb A1c by living a healthier lifestyle and making changes to your diet and exercising more
If you want to learn more about diabetes, we have dedicated information pages:
Frequently Asked Questions
What is the HbA1c test?
The HbA1c test measures the percentage of haemoglobin with glucose attached, providing an estimate of your average blood glucose over the past three months. It does not require fasting and is used to diagnose and monitor diabetes.
What is haemoglobin?
Haemoglobin is the iron-containing protein inside red blood cells that carries oxygen throughout the body. HbA1c measures how much of this protein has glucose attached to it.
What do different HbA1c readings mean?
Higher HbA1c reflects higher average glucose. Typical interpretation: below 5.7% is often considered normal, 5.7%–6.4% indicates prediabetes, and 6.5% or above on two separate tests can indicate diabetes. Your clinician interprets results in context.
What are the complications of type 2 diabetes?
Type 2 diabetes can affect the heart, brain, eyes, kidneys, and nerves. Because glucose may be elevated for years before diagnosis, some people already have complications at the time they are diagnosed. High glucose, high blood pressure, and abnormal lipids all increase risk.
What are macrovascular complications of diabetes?
Macrovascular complications involve large blood vessels. These include coronary artery disease (heart attack), cerebrovascular disease (stroke), and peripheral artery disease affecting blood flow to the legs.
What are microvascular complications of diabetes?
Microvascular complications affect small vessels and include retinopathy (eye disease), nephropathy (kidney damage), and neuropathy (nerve damage). These conditions often develop slowly and may not cause symptoms early on.
Is HbA1c linked to long-term diabetes complications?
Yes. Higher HbA1c levels are strongly associated with increased risk of both microvascular and macrovascular complications. Safely lowering HbA1c to your individual target reduces the likelihood of developing complications.
How can I lower my HbA1c and reduce complication risk?
Strategies include improving diet quality, reducing carbohydrate load, increasing physical activity, taking medications as prescribed, monitoring glucose as advised, and working with your healthcare team to adjust treatment toward your personal target.